Occupational health physicians remain the only medical specialists in the HSE without consultant status – but could a new taskforce mark the way forward? Catherine Reilly reports
Consultant status for occupational health physicians (OHPs) will be examined as part of an “occupational health taskforce”. However, any progress will require “separate detailed negotiations” between the HSE and IMO, an Executive spokesperson told the Medical Independent (MI).
OHPs are the only specialist-trained physicians in the HSE without consultant status. In 2021, the IMO and health management reached an agreement on consultant status for public health specialists after a 20-year dispute.
OHP role
According to a paper by the RCPI Faculty of Occupational Medicine (FOM), OHPs “combine their clinical acumen” with their knowledge of the workplace to “preserve and promote the health and wellbeing of the workforce”. OHPs undertake fitness for work assessments, sickness absence management, health promotion, and health surveillance, among other duties.
“OHPs recognise that the workplace is an important determinant of ill health and understand the hazards in the workplace which may be physical, chemical, biological, ergonomic, psychological, or environmental. The need for OHPs who can identify and respond to health concerns within the work environment has been acutely highlighted by the recent pandemic.”
The HSE is the State’s largest employer and employees deliver a diverse range of functions – from direct clinical care and laboratory services to administration, engineering, catering, and driving, for example.
Healthcare workers are exposed to various occupational hazards. These include exposure to violence, harassment, and traumatic events; ergonomic hazards from lifting loads and prolonged standing; exposure to biological and chemical agents; and physical hazards such as falls and ionising radiation.
OHPs in the public health service must hold specialist registration with the Medical Council. In Ireland, higher specialist training (HST) is delivered through the FOM and funded by the HSE. Entrants to the four-year HST programme must have completed basic specialist training or be qualified GPs. These requirements are similar to those in other medical specialties which have consultant recognition.
In 2010, the OHP role was reviewed as part of an IMO/HSE process. The review by the Hay Group found OHPs and medical consultants had “a similar minimum level of knowledge and experience” and encountered “a similar level of problems to solve to achieve a similar accountability”. However, the matter did not move forward. In 2021, the Department of Health confirmed that consultant status was under consideration. In June 2025, however, it described the issue as “not currently being considered within the Department”.
In its response in June, the Department added: “The pay position of occupational health physicians was reviewed in the context of the sectoral bargaining provisions under the Building Momentum, Public Service Agreement (PSA), which concluded on 31 December 2023. The revised salary scale provided for a 28 per cent increase in salary for occupational health physicians. This was in addition to the general pay rises outlined in the PSA 2024-2026.”
As OHPs represent a small specialty, the financial implications of consultant status would be relatively modest. However, at an individual level, the pay differential is substantial. The first point on the HSE OHP pay-scale is €171,878 compared to €231,215 under the 2023 consultant contract. But the concerns around consultant status go well beyond remuneration. Many specialists believe lack of parity impacts their professional standing within healthcare settings.
Specialists who spoke to MI expressed guarded feelings on the prospect of a taskforce. There was a suggestion it would merely serve to defer a resolution once again.
The specialty has lacked a strong collective voice on consultant status. The number of OHPs in healthcare is small and many public healthcare organisations have outsourced some provision to private companies. FOM boards have reflected the cross-sectoral employment settings of doctors – likely inhibiting a singular focus on consultant status in the HSE. Some specialists expressed disillusionment with the FOM and IMO for not advocating harder. In recent years, the FOM has been more active in promoting the value of occupational medicine to society – including the issue of consultant status.
Taskforce remit
The taskforce was established following an external review of HSE occupational health services conducted by a consultancy firm. Its role is to “implement the recommendations of the external review”, according to the HSE.
The taskforce is chaired by management consultant Mr Pat Harvey, former CEO of the North Western Health Board. The membership includes representatives from occupational medicine, nursing, administration, trade unions, and senior management.
The taskforce’s remit includes reviewing and validating “governance design options” for services and agreeing on the preferred option under the health regions’ structure. It will agree on a clinical operating model with “clear” team roles and responsibilities and career pathways, etc. It will also need to achieve a consensus on roles and responsibilities “in clinical situations involving, for example, public health and microbiology, whereby there may be interdependencies”.
The taskforce will “engage” with stakeholders on consultant status. However, progressing this matter will require a separate process, according to the HSE.
An IMO spokesperson said consultant status is “vital” to advance occupational health services.
“Other jurisdictions, notably the UK, have long established and recognised the role of consultant occupational health physician and in order to maximise the benefits and governance of this specialty, it is vital that Ireland follows suit,” outlined the IMO’s spokesperson.
“Following completion of [the taskforce], the IMO expects that a separate industrial relations process will need to be established between the IMO and HSE to advance the consultant status issue.
“Many of the issues within occupational health stem from the lack of a clear directorate structure as is the case in other specialties and areas of the health service. This structure on the medical side consists of a team of consultants reporting into a clinical director and occupational health should be no different to any specialty in this regard.”
Many of the issues within occupational health stem from the lack
of a clear directorate structure…
‘Critically low’
The HSE Workplace Health and Wellbeing Unit (WHWU) is the ‘central governance unit’ for the HSE occupational health departments. The current WHWU Director is Dr Grant Jeffrey, a specialist in occupational medicine. The WHWU is part of the human resources (HR) directorate and reports to Chief People Officer Ms Anne Marie Hoey.
In 2022, a HSE corporate risks report noted a “critical short supply” of occupational health staff nationally and internationally. During 2024, the HSE recruitment embargo exacerbated staffing issues. The wide net of the embargo entangled OHP posts in spite of an exemption for consultants. Staffing deficits impacted on the capacity to deliver core functions, leading to system-wide consequences.
In an internal email in June 2024, Ms Hoey referenced a discussion with the HSE CEO on the “critically low” levels of nurse staffing in occupational health departments and the “resultant pressure on their service delivery”, according to records obtained under Freedom of Information (FoI) law. The CEO agreed to derogate 10 whole-time equivalent (WTE) nursing posts, stated Ms Hoey’s email. Records also showed Dr Jeffrey sought OHP and nurse derogations in order to deliver “safe and effective” occupational health services.
In its FoI response in late 2024, the HSE declined to release details of expenditure on OHP services provided by private companies during 2023 and 2024, citing commercial sensitivity. The HSE also refused to release WHWU records on waiting times, arguing these related to deliberative processes.
In HSE services, 15.1 WTE OHPs are in post and there is one vacancy. There are 45.7 WTE nurses in post and five vacancies. “Recruitment is underway for approved vacancies,” said its spokesperson.
In relation to management referrals, as of June 2025, the national average time to first appointment was eight weeks for routine referrals – ranging from one to 16 weeks. Urgent referrals were prioritised and assessed “as soon as possible”. Regarding pre-placement health assessments, the average time for an “occupational fit slip” to be issued was two weeks – ranging from one to eight weeks.
The spokesperson added: “It is necessary to have some outsourced services, which are procured in line with public procurement, to supplement occupational health services. The use of outsourcing remains under active monitoring and review.”
Advocacy
The recruitment embargo prompted significant advocacy by occupational medicine SpRs. In April 2024, SpRs wrote to the Minister for Health expressing deep concerns over the impact of the embargo and wider issue of consultant status.
“Many of us are considering moving permanently to the UK and further abroad where we will be recognised as consultants, and not face impediments to our employment in the public health service. Others are considering retraining in a different specialty,” according to the letter.
The correspondence regretfully advised that many SpRs would not have trained in the specialty if they had known they would not receive consultant status.
The correspondence provided stark insights into the detrimental impact of staffing shortages on staff and patients. “HSE policy dictates that HSE staff require an occupational health physician review in numerous different circumstances. Some examples of this include staff members who have been on long-term sickness absence, those who are injured or assaulted at work or those who are critically unwell. Current waiting times for appointments with an OHP are significant, many staff members are waiting six weeks or more to be seen.”
The knock-on effects could not be underestimated, according to the letter.
Lack of access to timely OHP appointments reduced the likelihood of staff returning to meaningful employment. This negatively affected outcomes for staff and compounded staffing difficulties.
RCPI
Following this advocacy, the RCPI issued strong comments to MI in support of consultant status.
According to the statement by RCPI President Dr Diarmuid O’Shea and the then FOM Dean Dr Sheelagh O’Brien, “immediate action” was required to ensure occupational medicine specialists were accorded consultant status in the Irish health service.
Their statement said the FOM continued to advocate for this recognition.
In July 2024, the RCPI’s Priorities for Health for the Next Government included consultant status for occupational medicine specialists as a key priority.
Asked for an update on its engagement with the Department, an RCPI spokesperson said: “We don’t have any update on the consultant status in this speciality, which is included in our manifesto document for the new Government. In terms of intake to the specialty, three doctors have joined the Faculty of Occupational Medicine Programme this year. The scheme is full, with 14 people currently on programmes. There has been no attrition in the last 24 months.”
However, while the RCPI reported the scheme as “full”, the number of places has remained relatively static. MI requested an interview with the current FOM Dean Dr Alex Reid, but he was unavailable on this occasion.
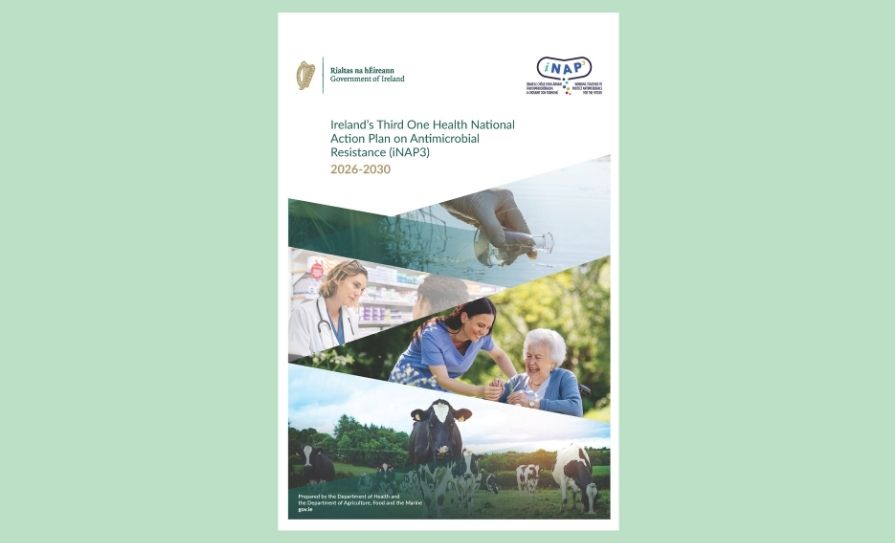
HSA healthcare advisory committee publishes action plan
Data on workplace-related violence and aggression should be analysed to develop focused interventions, according to the Health and Social Care Advisory Committee (HSCAC) Action Plan 2025–2027.
The HSCAC was established by the Health and Safety Authority (HSA) at the end of 2023. The committee comprises employer, regulatory and healthcare union representatives. Its role is to advise and support the HSA in promoting occupational health and safety in the health and social care sector. Its action plan was published earlier this month.
In 2024, the sector accounted for 13.7 per cent of all employed persons. The sector reports the highest number of non-fatal work-related incidents to the HSA, with falls, manual handling, and work-related violence and aggression the leading “incident triggers”.
The HSCAC has identified five key goals to support the HSA’s work:
- Enhance information and intelligence to inform interventions.
- Promote a positive health and safety culture in the workplace.
- Promote and support safety representatives and safety consultation in health and social care workplaces.
- Undertake initiatives to reduce the risk of injury to employees from work-related violence and aggression.
- Enable employers and employees to implement best practice in managing the risk of work-related psychosocial hazards, in particular work-related stress and work-related bullying.
According to the document: “The critical success factors for achieving the objectives include the level of engagement by external stakeholders and the availability of resources to support the implementation of the action plan.”
Mr Mark Cullen, interim HSA Chief Executive Officer, commented: “Prioritising the safety, health, and welfare of this essential workforce is not just a legal duty – it is a societal imperative. The work of the HSCAC will be vital in guiding our regulatory and promotional efforts over the next three years.”
A HSE spokesperson said: “The HSE is a member of the health and social care advisory committee to the HSA and is pleased to contribute to their strategy which aligns with the HSE’s occupational safety and health work plans. These plans include supporting the review of the HSE’s Incident Management Framework, supporting consultation with our 900+ safety representatives, and supporting pillar two of the Healthy Workplace Framework – The Psychosocial Work Environment.”









Leave a Reply
You must be logged in to post a comment.