Reference: November 2025 | Issue 11 | Vol 11 | Page 39
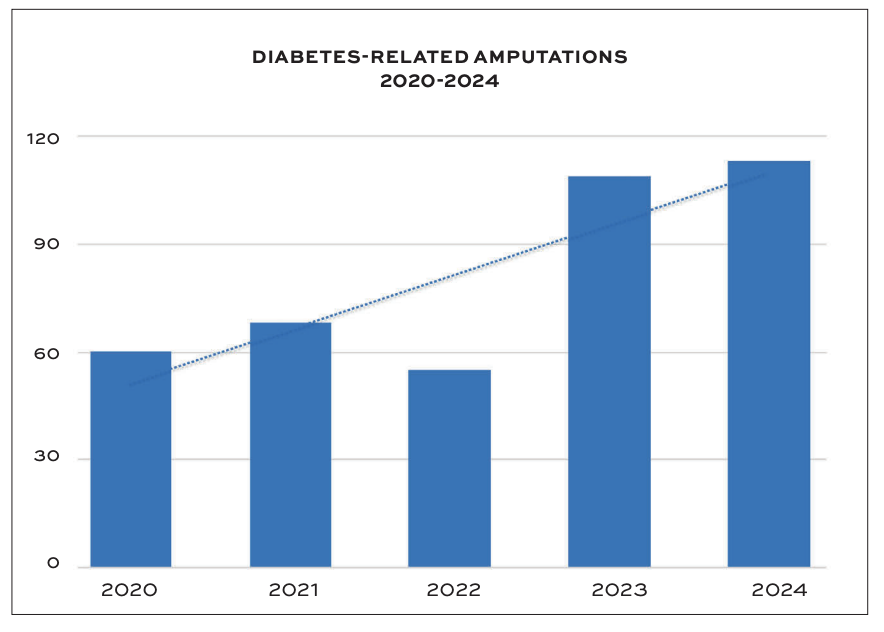
Diabetic foot disease amputations are one of the most distressing and preventable outcomes of this chronic disease. The common misconception is that these outcomes only occur in uncommon or extreme cases. Yet, a major tertiary hospital has recorded an 88 per cent increase in diabetic foot amputation rates over a five-year period (Figure 1).
This mirrors the current climate in Ireland, with a rising prevalence in diabetes affecting more than 250,000 people.1 This places further strain on community and tertiary-based services, where staff funding and provisions have remained largely static.
The cost of a diabetic foot amputation is not just the loss of mobility for the patient. It is associated with a high mortality rate – five years after a diabetic foot amputation, the mortality rate exceeds 70 per cent.2 Also, it is estimated that major and minor diabetic foot amputations each cost the health service €60,000 and €30,000, respectively.3
Within these statistics, there is the uncomfortable truth that with adequate access to an appropriate provision of care, diabetic foot amputations are largely regarded as avoidable. When podiatrists are adequately resourced and integrated into multidisciplinary teams, international evidence shows major amputation rates can be reduced by up to 85 per cent.4,5 This brings up the question – what is happening in the Irish landscape?
The Irish landscape: Podiatry and diabetic foot disease
The National Model of Care for the Diabetic Foot calls for equitable access to podiatry services across all Community Health Organisations (CHOs) in Ireland, with the goal of delivering preventative care and reducing the rates of progression to active diabetic foot disease.3
In principle, this strategy should shift the burden away from acute hospital services by intercepting complications earlier. However, the initial investment in the Diabetic Foot Model of Care has been insufficient to meet the escalating demand. Implementation has been constrained by workforce shortages, recruitment challenges, and inconsistent engagement across CHOs.6
Evidence shows that many podiatrists in Ireland are unable to deliver the full scope of care envisaged under the model due to excessive caseloads and inadequate staffing, particularly within acute hospital settings.6,7 In some areas, patients with active diabetic foot disease are not being reviewed within the recommended 24-48 hours, highlighting systemic strain and inability to access key services.7
The broader problem in these integrated care initiatives is that it often depends on local leadership, resources, and existing structures, rather than a uniform national rollout, leading to variation and fragmented service delivery.8
The consequences of inadequate preventive capacity place a significant financial burden on the healthcare service, as the cost of managing severe diabetic foot complications in hospital settings far exceeds that of early community-based intervention.
An Irish economic analysis estimated that individuals with diabetic foot ulcers incurred an average cost of €9,566 over 18 months, compared with €2,785 for those without ulcers; a 175 per cent increase.9
Evidence from the UK suggests that improving community podiatry staffing levels and resources directly reduces hospital admissions for diabetic foot disease.10 The failure to adequately invest in and scale podiatry services has resulted in preventable cases progressing to severe disease, placing unsustainable pressure on acute hospital systems and increasing the financial burden on the health service.
Regression analysis: Podiatry staffing and emergency amputations
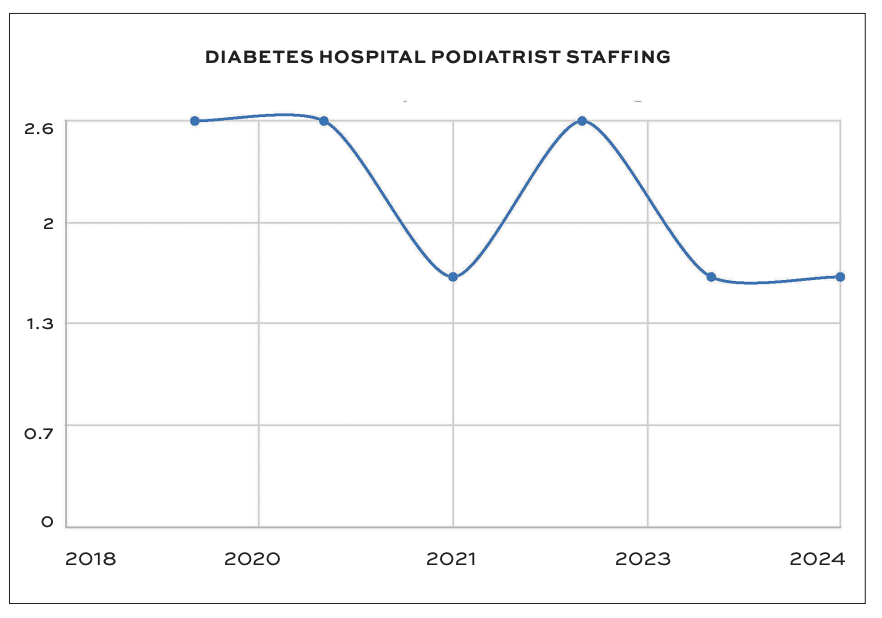
Between 2020 and 2024, a major tertiary hospital recorded 405 diabetes-related amputations, an 88 per cent increase over five years. Yet during the same period, podiatry staffing remained unchanged, as did the investment in the hospital diabetic foot service.
It was also noted that, during this time, the service was staffed by 1.6 podiatry whole-time equivalents (WTE), with a vacant post the majority of the time, servicing a catchment area exceeding half a million people.
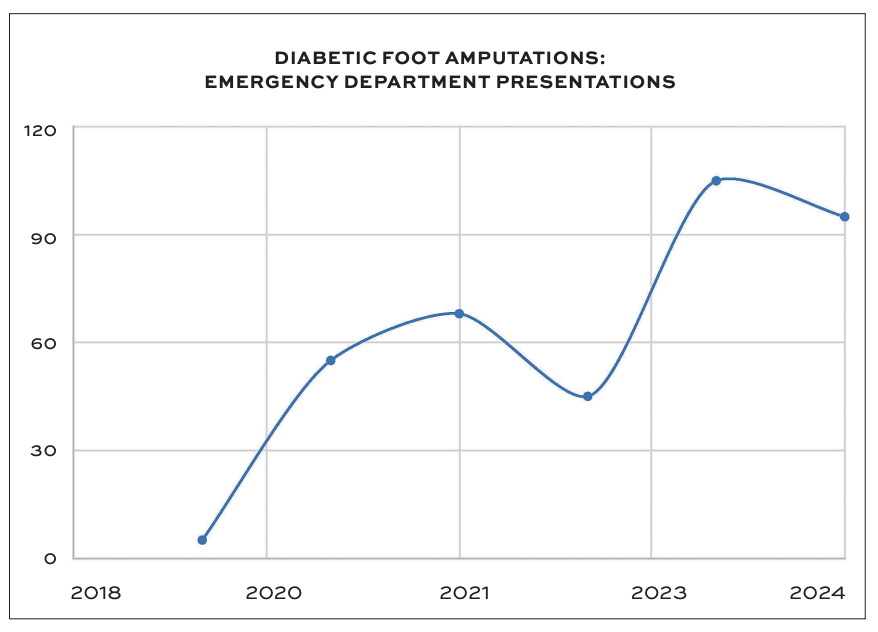
A regression analysis demonstrated a significant relationship between hospital podiatry staffing and emergency department presentations for diabetic foot disease resulting in amputation (R² = 0.67, p = 0.045) (Figures 2-4). This means that approximately two-thirds of the variation in emergency presentations can be linked to podiatry staffing levels.
For every one additional WTE podiatrist, the number of emergency presentations requiring amputation can decrease by around 54 cases over a five-year period. The negative coefficient demonstrates that higher podiatry staffing is consistently associated with fewer emergency amputations.
This correlation highlights the tangible impact of workforce capacity on patient outcomes. Arguably, the findings reinforce the notion that diabetic foot complications are not inevitable, but are largely a reflection of system design and investment priorities.
Looking forward
The findings from this tertiary hospital reflect a national challenge – without sustained investment in community and acute diabetic foot services, preventable amputations will continue to rise. The 2021 National Model of Care offers the correct foundations for this; however, the delivery has been constrained by workforce shortages, inconsistent implementation, and lack of ring-fenced funding for the diabetic foot.
To achieve meaningful change, investment must focus on expanding and retaining podiatry posts across all CHOs, ensuring that every hospital has a fully staffed multidisciplinary diabetic foot team and standardised rapid referral pathways for high-risk patients.
A national audit and benchmarking for diabetic amputation rates, ulcer healing, and emergency attendance should be prioritised to track performance and accountability.
Ultimately, the success of Ireland’s diabetic foot strategy will depend on turning policy into practice, improving resources, increasing key personnel and coordination required to prevent avoidable limb loss.
Recommendations
The following recommendations align with the National Model of Care for the Diabetic Foot3 and international best practice standards, addressing current deficits in workforce, governance, and service integration.
| REGRESSION STATISTICS | |
|---|---|
| Multiple R | 0.821547118 |
| R Square | 0.674939667 |
| Adjusted R Square |
0.593674584 |
| Standard Error |
23.09040205 |
| Observations | 6 |
| ANOVA | ||||||||
|---|---|---|---|---|---|---|---|---|
| df | SS | MS | F | Significance F | ||||
| Regression | 1 | 4428.166667 | 4428.166667 | 8.30540794 | 0.044926692 | |||
| Residual | 4 | 2132.666667 | 533.1666667 | |||||
| Total | 5 | 6560.833333 | ||||||
| Coefficients | Standard Error | t Stat | P-value | Lower 95% | Upper 95% |
Lower 95.0% |
Upper 95.0% |
|
| Intercept | 176.2666667 | 40.69853942 | 4.331031756 | 0.01233968 | 63.2694061 | 289.2639 | 63.26941 | 289.2639 |
| X Variable 1 | -54.33333333 | 18.85323432 | -2.881910467 | 0.04492669 | -106.6783035 | -1.98836 | -106.678 | -1.98836 |
FIGURE 4: Regression analysis podiatry and diabetic foot Emergency Department presentations
1. Secure sustained investment in diabetic foot services
Funding for the Model of Care has been insufficient to support national implementation. Without ring-fenced budgets, diabetic foot services are often deprioritised at both community and acute levels.3,8 Dedicated, multi-annual investment is required to expand community-based podiatry capacity, maintain hospital multidisciplinary teams, and enable rapid-access clinics for high-risk patients. International evidence demonstrates that structured, well-funded diabetic foot pathways significantly reduce amputation rates and hospital admissions.5,11
2. Expand and retain the podiatry workforce across hospitals and CHOs
The shortage of podiatrists remains the single most critical barrier to preventative care delivery. Recruitment should be accompanied by measures to improve retention, including defined career progression pathways, competitive remuneration, and opportunities for advanced clinical practice roles. Further investment in educational institutions offering podiatry courses would help overcome the skills shortage that is currently seen in the job market.
3. Ensure every acute hospital has a fully staffed multidisciplinary diabetic foot team
Hospitals without dedicated multidisciplinary diabetic foot teams experience higher rates of emergency admissions and amputations.5 A standalone budget should be provided to staff who run diabetic multidisciplinary diabetic foot
team foot services.
4. Implement a National Diabetic Foot Audit and performance benchmarking
A centralised audit programme should track key indicators including ulcer healing rates, amputation incidence, time to assessment, and hospital length of stay. Public reporting and benchmarking across CHOs and acute sites would enhance transparency, accountability, and quality improvement.5
References
- Health Service Executive. Chronic disease management programme: Diabetes. Dublin: HSE; 2021. Available at: www.hse.ie/eng/services/list/2/primarycare/chronic-disease-management-programme/.
- Jeffcoate WJ, Harding KG. Diabetic foot ulcers. Lancet. 2003;361(9368):1545-1551. doi:10.1016/S0140-6736(03)13169-8.
- Health Service Executive. National model of care for the diabetic foot. Dublin: HSE; 2021. Available at: https://www.hse.ie/eng/about/who/cspd/ncps/diabetes/moc/.
- Paisey RB, Abbott A, Paisey CF, Walker D. Diabetic foot ulcer incidence and survival with improved diabetic foot services: An 18-year study. Diabet Med. 2019;36(11):1424-1430. doi:10.1111/dme.14045.
- Kerr M, Barron E, Chadwick P, et al. The cost of diabetic foot ulcers and amputations to the National Health Service in England. Diabet Med. 2019;36(8):995-1002. doi:10.1111/dme.13973.
- O’Neill S, O’Keeffe N, Collins A, Cullen W. A realist evaluation of a national model of care for the diabetic foot in Ireland. International Journal of Integrated Care. 2017;17(5):1-8. https://doi.org/10.5334/ijic.3489.
- Barry, C. Challenges in delivering diabetic foot care in Ireland: A workforce perspective. [Unpublished conference presentation]. Health Service Executive; 2023.
- Pallin JA, Buckley-O’Farrell K, Riordan F, et al. Implementing an integrated diabetic foot care programme in Ireland: Podiatrists’ experience. BMC Health Serv Res. 2023;23(1):1157. Published 2023
Oct 26. doi:10.1186/s12913-023-10144-z. - Gillespie P, O’Shea E, Smith SM, O’Dowd T. The effect of foot ulcers on costs of care for people with diabetes in Ireland. The Diabetic Foot Journal. 2014;17(3):107-121.
- Paisey RB, Abbott A, Levenson R, et al. Diabetes-related major lower limb amputation incidence is strongly related to diabetic foot service provision and improves with enhancement of services: Peer review of the south-west of England. Diabet Med. 2018;35(1):53-62. doi:10.1111/dme.13512.
- Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. N Engl J Med. 2017;376(24):2367-2375. doi:10.1056/NEJMra1615439.
