A clinical overview of the diagnosis, treatment and management of osteoporosis
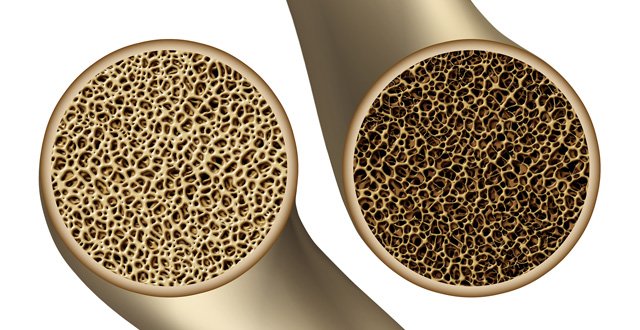
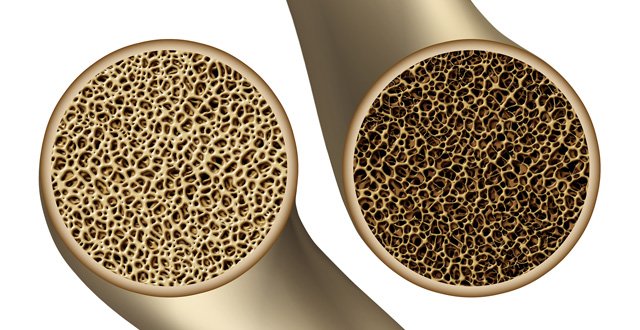
A person will develop osteoporosis when
more bone is lost than is formed. This results in low bone mass and compromised
bone strength, with an increased risk of fracture. The majority of these
fractures are preventable. The most common bones to fracture are the hip, spine
and wrist, however it can affect any bone. All low-trauma fractures should be
considered osteoporosis, unless proven otherwise, even when the patient has
fractured bones from a fall on ice or cement.
One
fracture doubles the risk of further fractures and untreated osteoporosis leads
to pain, disability, loss of independence and premature death. Osteoporosis is
the commonest bone disease worldwide and there are no signs or symptoms prior
to fracture.
Prevention
More women die from the complications
of osteoporotic fractures than from all cancers of the ovary, uterus and cervix
put together.
While it
is more prevalent in post-menopausal women, it should not just be considered an
older woman’s disease, as more men die as a result of osteoporosis than get
prostate cancer. Men are more likely than women to die after fracturing a hip
and also to require care in a long-term facility.
One-in-two
women and one-in-four men over the age of 50 years will develop an osteoporotic
fracture in their lifetime, if they do not look after their bone health.
About 20 per cent of people aged 60+ who fracture a hip
will die within six-to-12 months, due to the secondary complications of the
fracture, which are blood clots, pneumonia or infection from being bed-bound.
About
half (50 per cent) of people aged 60+ who fracture a hip will no longer be able
to dress, wash or walk unassisted.
Only 30
per cent of people aged 60+ who fracture a hip will regain their independence.
It is
never too late to start a bone-healthy exercise programme, even if a person has
already been diagnosed with osteoporosis or are at high risk of developing
osteoporosis. However, those with bone loss (osteopaenia/osteoporosis and
osteoarthritis) should not be encouraged to do yoga exercises/stretches
(sit-ups, twisting of the spine, touching toes with legs straight) that involve
forward flexion or high-impact exercises such as bone-loading due to the risk
of fracture. These patients should be advised to avoid bending forward. These
patients will be doing some flexion when dressing, etc. High-impact exercise
should be encouraged in children, teenagers and young adults who do not have
risk factors for bone loss. Research shows that weight-bearing exercise,
especially right before puberty, can significantly improve bone density. Dancing
is excellent for bones due to the variety of weight-bearing.
Every
health professional should be screening their patients/clients for risk factors
for bone loss. Any patient with a low trauma fracture should be assessed for
their risk of bone loss.
NOTE: There has been a marked increase in
the stress levels of both males and females, due to either excess psychological
or physiological stress. Cortisol is released in response to stress. High
levels of cortisol reduce both oestrogen in females or testosterone in males,
causing increased bone loss. High cortisol increases RANKL and the formation of
osteoclasts, which increase bone loss. It takes three weeks to lose bone, but
three months to replace the lost bone.
Elevated
levels of cortisol cause calcium depletion of bone tissue. Cortisol mainly acts
on the outer layer of the bone called the periosteum. Elevated cortisol
inhibits osteoblastic activity and cell proliferation, which reduces bone
formation, resulting in reduced bone density and placing the patient at risk of
fractures.
Diagnosis
Postural changes (loss of height, head
forward from body, shoulders rounded, hump developing on back) are commonly
thought of as the natural ageing process, when they are the biggest red flag
for possible undiagnosed vertebral fractures. About 75 per cent of those with
vertebral fractures have intermittent back pain; only 25 per cent have constant
pain.
A DXA
scan of the spine and hips is the gold standard for diagnosing osteoporosis and
is the only test that the Irish Osteoporosis Society (IOS), who are the
national experts on osteoporosis, recommend. A DXA scan is a simple, painless
test that takes approximately 15 minutes and is not claustrophobic. A DXA scan
involves a 10 per cent radiation level of a regular chest x-ray.
NOTE: The IOS does not recommend the use of
ultrasound scanning of the forearm, heel or tibia for screening or diagnosing
bone loss. The IOS does not recommend the Fracture Risk Assessment Tool (FRAX),
as there are only 12 risk factors on it and there are approximately 200 risk
factors for bone loss.
A T score
compares an adult’s results with the mean peak bone mass of a large number of
normal females and males between the ages of 20-to-40 years.
A Z score
compares the patient’s score with their own age group; this is usually used in
the diagnosis of the spine in children and adolescents (aged under 21 years).
Their bone age should also be compared to their chronological age, by x-raying
the carpal bones of their non-dominant hand.
NOTE: T scores and Z scores are the same
between 20 and 40 years.
Mild osteopaenia is a T score of -1 to -1.49.
Moderate osteopaenia is a T score of -1.5 to -1.9.
Marked osteopaenia is a T score of -2 to -2.49.
Osteoporosis is a T score of -2.5 to -2.99.
Severe osteoporosis is a T score of -3 or higher.
Research
shows that the majority of fractures happen in the moderate to marked
osteopaenia range.
The T
score of each vertebra should be included in the report, not just the average
of the four. If a vertebra is more than one standard deviation better than the
vertebra with the lowest T score, it should be excluded from the average score.
This false higher reading may be due to increased density due either to
osteoarthritis or to a vertebral fracture.
Examples
of DXA results with false higher readings:
T score
of L1 = -3.4 = Severe osteoporosis.
T score
of L2 = -3.0 = Severe osteoporosis.
T score
of (L3) = -1.9 = Moderate osteopaenia = false higher reading.
T score
of (L4) = -2.0 = Marked osteopaenia = false higher reading.
The
average of the T scores above, prior to elimination = -2.7
L3 and L4
should be eliminated, which is when you should see brackets around the results;
unfortunately, this is not always done.
Therefore,
after elimination, the average T score = -3.2. This shows that a person could
be told they have osteoporosis, when they actually have severe osteoporosis. A
diagnosis should not be made just on the total average of either the spine or
the hip.
NOTE: If only two vertebrae are left,
because the other vertebrae have been eliminated or both hips have been
excluded because of hip replacements, then a lateral vertebral assessment (LVA)
— a DXA of the mid and upper back or lateral thoracic x-ray — should be done.
If a
person has developed a ‘Dowager’s hump’, loss of height, postural changes, or
scoliosis, back pain, an LVA is recommended. An LVA is usually not done unless
specifically requested on the referral form.
If LVA is not available, a lateral x-ray of the spine is
advised. This will show if the shape of the bones in this area is compressed
due to osteoporosis fractures. However, this cannot be used to monitor the
patient’s response to treatment in this area.
Treatments
All treatments should be prescribed on
an individual basis.
The menopause is only one of 200 causes and men do not go
through the menopause! Bones need normal sex hormones, adequate calories and
protein, vitamin D, calcium and fluids (1.5 litres), and appropriate, regular
weight-bearing/strengthening exercise to keep them healthy. Stress, low sex
hormone levels, family history, gluten sensitivity and medications/treatments
causing bone loss are some of the many risk factors.
The
causes of bone loss should never be assumed; they should be investigated and
addressed. This is done by an extensive bone health questionnaire and extensive
blood tests. Both can be requested from the IOS: info@irishosteoporosis.ie.
Bisphosphonates,
ie, alendronic acid, and teriparatide and denosumab are all options for women
and men. HRT and the pill are options for women. There are contraindications
for all treatments and especially premenopausal women.
NOTE: Those with gastrointestinal disorders
usually have difficulty taking bisphosphonates, which can decrease compliance
levels.
NOTE: All patients need normal vitamin D,
cortisol, calcium, PTH and renal function and appropriate weight-bearing
exercise to get the maximum benefit from all treatments.
Situation in Ireland
There are approximately 280,000 people
in Ireland who have undiagnosed osteoporosis, and of the 15 per cent diagnosed,
only 5 per cent are put on a treatment. In the vast majority, 95 per cent, of
people who contact the national osteoporosis helpline (01 637 5050), causes of
bone loss have been assumed.
The low diagnosis rate of osteoporosis results in
patients with low trauma fractures blocking hospital beds and with our ageing
population, this is going to significantly affect our overstretched capacity
issues and the quality-of-life of those affected. This is the reason why FLS
(Fracture Liaison Services) are urgently needed in Ireland. An FLS is when a
dedicated co-ordinator acts as the link between the patient and all other
departments in a hospital, including primary care physicians. One hip fracture
costs the state €55,000 in total and there are over 3,000 hip fractures a year,
therefore FLS are essential.
If current trends continue, it is estimated that costs
will be: €922 million-€1.077 billion by 2020 and €1.587-€2.043 billion by 2030.
Remember, osteoporosis is preventable
as well as treatable in the majority of people.




Leave a Reply
You must be logged in to post a comment.