Reference: August 2025 | Issue 8 | Vol 11 | Page 22
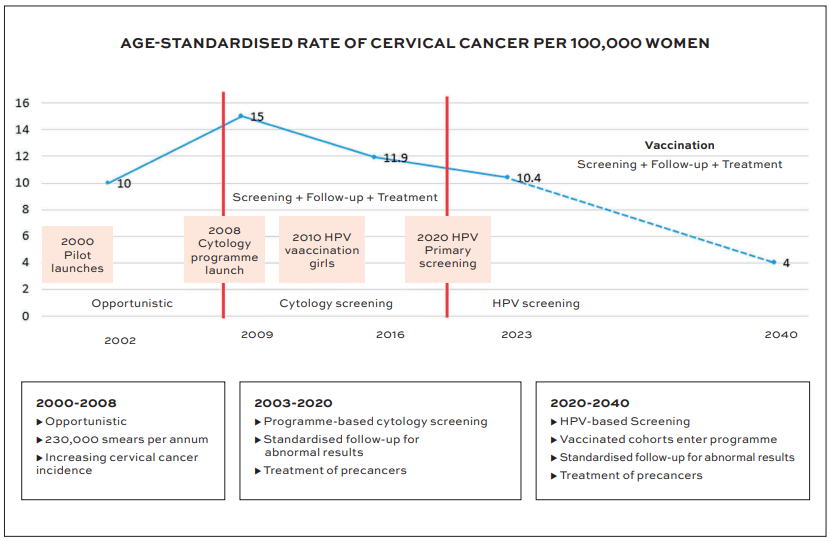
Ireland is on track to eliminate cervical cancer by 2040. The WHO defines elimination of cervical cancer as reaching an incidence lower than four cases per 100,000 women, making cervical cancer a rare disease and eliminating it as a public health problem. Ireland’s incidence rate is now 10.1 per 100,000 women. This bold but achievable target is grounded in a cohesive, evidence-informed strategy that combines HPV vaccination, primary HPV screening, effective early treatment, and a strong commitment to equity and public trust.
The WHO has outlined a global strategy to eliminate cervical cancer this century, based on each country reaching the following 90-70-90 targets by 2030:
- 90 per cent of girls fully vaccinated with the HPV vaccine by age 15;
- 70 per cent of women screened with a high performance test by age 35, and again by age 45;
- 90 per cent of women with pre-cancer treated and 90 per cent of women with invasive cancer managed.
Ireland has embraced this framework as part of a national roadmap. From rebuilding confidence in HPV vaccination after a period of public scepticism, to leveraging the trusted role of GPs and general practice nurses in screening uptake, and strengthening colposcopy and cancer treatment pathways, the approach is both collaborative and inclusive. Scientific modelling, robust surveillance, and a commitment to quality assurance underpin every aspect of the strategy, with a clear focus on addressing disparities and ensuring no woman is left behind.
Our cancer elimination strategy is also supported by the Women’s Health Fund – a process of investment under the Women’s Health Action Plan 2024-2025, which commits to taking action to improve the health outcomes for women and girls across the country. The level of support our strategy is receiving from healthcare, advocacy, community, and Government is positioning Ireland not only to meet the WHO targets, but to become a global leader in making cervical cancer a rare disease.
Nevertheless, reaching elimination will require sustained commitment and coordination between the CervicalCheck programme, primary care, colposcopy services, laboratories, the National Immunisation Office (NIO), and other areas of the HSE.
Most importantly, elimination will only be achieved by engaging and working with public and patient partners in civic society, including women, girls, and the men who love and support them. This article outlines how these elements come together within our strategy, and how shared effort over the next decade could transform population health outcomes for generations to come.
Organised screening
Cervical cancer remains a significant public health concern in Ireland, with approximately 250 women being diagnosed each year and 80 women dying from this disease annually.1 Over 75 per cent of the 1.33 million women who are eligible for cervical screening attend. This is a high level of population coverage by international standards placing Ireland third among Organisation for Economic Co-operation and Development (OECD) countries for the highest coverage.2,3
Prior to 2008, cervical screening in Ireland was opportunistic, inconsistent, and largely unregulated. There was no centralised call/recall system, and follow-up of abnormal results was often fragmented. In 2002, turnaround times for results ranged from one to 13 weeks, and quality assurance varied widely across laboratories processing screening tests. By 2007, some women were waiting more than six months for the results of their smear test. Many women were either under-screened or over-screened, contributing to preventable cases of cervical cancer.4,5
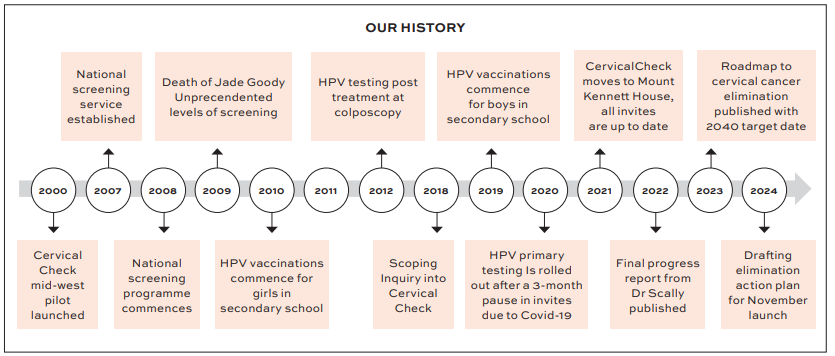
The establishment of CervicalCheck in 2008 marked a watershed moment in public health, bringing a free population-based, cervical screening programme. Initially targeting women aged 25-60 with regular invitations every three years for ages 25-44 and every five years for 45-60, the programme brought structured oversight, consistent follow-up, centralised data monitoring, and quality assurance across the full pathway from sample-taking through the laboratory and colposcopy services. This shift quickly led to a measurable decline in cervical cancer incidence and mortality, with quality assurance and accessibility as key pillars of the model.5,6
Ireland’s shift to HPV primary screening in March 2020 was grounded in strong clinical evidence and marked a major advancement in the national cervical screening programme. Studies show that over 90 per cent of cervical cancers are caused by persistent infection with high-risk HPV types and that HPV testing is significantly more sensitive than cytology in detecting high-grade cervical intraepithelial neoplasia (CIN).7,8 A negative HPV test also offers superior long-term reassurance.
One large study found the three-year risk of developing high-grade CIN following a negative HPV test was 1.21 per 1,000, compared to 4.52 per 1,000 for a negative cytology result.9
In response to this evidence, Ireland became one of the global leaders in cervical cancer prevention by adopting HPV testing as the first-line screening tool. This required a substantial shift in clinical messaging and an enhanced focus on sample-taker education.
The HSE National Screening Service programme includes:
- CervicalCheck programme team;
- 1,900 clinically responsible doctors (GP contract holders);
- Over 4,000 registered sample-takers;
- Two screening laboratories;
- 15 colposcopy units;
- 12 histology laboratories.
This robust infrastructure ensures consistent quality, rapid turnaround times, and a strong emphasis on putting women’s needs and understanding at the centre of care.
As anticipated, the enhanced sensitivity of HPV testing led to a temporary increase in colposcopy referrals – currently at 8-9 per cent of screened individuals, up from 4-6 per cent under cytology-based testing.2 Predictive modelling suggests this is a transitional phase and that as HPV vaccinated cohorts enter the screening programme, both referral and treatment volumes are expected to decline, improving programme efficiency and reducing the risk of overtreatment.10
This evolution closely aligns with the WHO’s global elimination strategy, which recommends that 90 per cent of women identified with cervical disease receive timely and appropriate treatment.7 Ireland is well-positioned to meet this benchmark. All women referred for colposcopy are offered an appointment, and in 2022/23, over 75 per cent of referrals were seen within the recommended waiting times: 85.9 per cent of women with high-grade abnormalities were seen within the target of four weeks and over 70 per cent of those with low-grade or normal results were seen within eight weeks.2
These outcomes reflect the effectiveness of Ireland’s evidence-based screening model, underpinned by strong clinical governance and continuous professional education. The Irish programme is an outlier internationally in its approach to commissioning the diagnostic arm, as well as the screening tests. This approach enables the programme to track the follow-up of abnormal screening tests and ensure that
women are not lost to follow-up.
Screening coverage
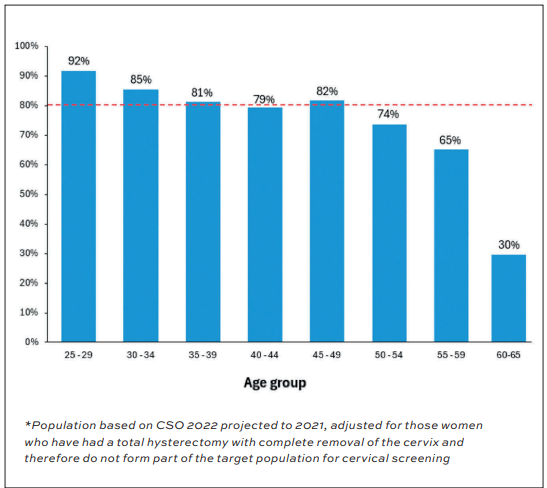
Screening coverage refers to the proportion of the eligible population who have a screening test under the programme within a defined period. It is a fundamental or base measure of a screening programme’s effectiveness in reducing the burden of disease and is internationally recognised as a core performance indicator. CervicalCheck aims to achieve at least 80 per cent population coverage over a five-year interval, in line with best practice guidelines.
Ireland continues to perform strongly by global standards. As reported in the 2022/23 programme data, CervicalCheck ranks third highest among OECD countries. The average OECD screening coverage is approximately 56 per cent, whereas Ireland is consistently above 75 per cent.
Engagement is particularly high among women aged 25-29 (92 per cent coverage), in contrast to trends observed in countries such as England, Canada, Sweden, and France, where this age group is typically the least likely to participate.
In the UK, for example, five-year coverage among women aged 25-29 declined from approximately 72 per cent to 65 per cent between 2005 and 2017.11 Single-invitation attendance among 25-year-olds in some regions, such as Manchester, has been reported as low as 30 per cent.12
However, coverage declines with age in Ireland. Participation among women aged 60 and above drops significantly, with the lowest uptake – around 30 per cent – seen in those aged 60-65 years. Various programme strategies to address this included a focus on older women in 2023 when women who had exited the cytology programme were offered a once-off HPV test. Additional education targeting post-menopausal women and sample-takers focused on making screening more comfortable and removing barriers to participation.
Sustaining and increasing coverage remains a national priority, particularly among under-screened groups. Given the strong correlation between high coverage and reductions in incidence and mortality, continued investment in accessibility, equity, and trust-building is essential.13
These efforts are not only pivotal for reaching underserved populations, but also for aligning with the WHO’s elimination strategy, which recommends that every woman receives at least two high-performance tests between 35 and 45 years of age. Ireland is well on its way. The latest programme data indicates that we are meeting this benchmark. This is a key milestone on the road to achieving cervical cancer elimination as a public health problem by 2040.
HPV vaccination
Ireland introduced school-based HPV vaccination for girls aged 12-13 years in 2010, accompanied by a catch-up programme for older adolescents. Initial uptake was high, reflecting strong public trust in HPV vaccination. However, by 2016, vaccine confidence had sharply declined due to groups spreading anti-vaccine misinformation and negative media coverage. Parental concerns were amplified by social media and mainstream media questioning vaccine safety and this further contributed to widespread vaccine hesitancy.14,15
In response, the HSE’s NIO, in collaboration with public health stakeholders, implemented a robust recovery strategy to rebuild trust and support informed decision-making. Key measures included:
- Direct engagement with parent groups to listen and respond to concerns.
- A temporary delay of the school-based programme to allow time for communication and reassurance.
- Enhanced transparency and improved educational resources, including a revamp of the www.HPV.ie website.
- Provision of WHO-accredited information on vaccine safety.
- Delivery of consistent, evidence-based messaging in partnership with the Irish Cancer Society and Trinity College Dublin research group CERVIVA.
In addition, the NIO adopted new recommendations from the National Immunisation Advisory Committee (NIAC) and the National Immunisation Technical Advisory Group (NITAG), including the introduction of a one-dose HPV vaccine schedule for people aged under 15 years. This change is grounded in WHO-endorsed evidence indicating similar effectiveness to the traditional two-dose schedule.13
One of the most important contributions to restoring public trust in HPV vaccination was the advocacy of the late Laura Brennan, a young Irish woman living with terminal cervical cancer. Her powerful and personal campaign supporting HPV vaccination resonated both nationally and internationally. Laura appeared in the RTÉ documentary This Is Me, helping reframe the narrative around HPV vaccination. Her advocacy is widely credited with restoring public confidence in HPV vaccination.14
Following these efforts, HPV vaccine uptake began to increase. In 2019, Ireland became one of the first countries in Europe to roll out gender-neutral HPV vaccination.16 From December 2022 to December 2024, the HSE offered a vaccination catch-up opportunity for those who did not receive the vaccine as part of the school programme.
The Laura Brennan HPV Vaccine Catch-Up Programme, named in Laura’s honour, continued this work up until 2024. It provided free HPV vaccines to over 3,500 young people who had missed the opportunity in school. The expanded programme included:
- All unvaccinated students from 2nd to 6th year in post-primary education;
- All unvaccinated males who had left school and were aged 21 or younger at the time of vaccination offer;
- All unvaccinated females who had left school and were aged 24 or younger at the time of offer.
As of 2023, Ireland’s HPV vaccine uptake had risen to 84 per cent, a significant public health milestone.17 However, continued effort is required to meet the WHO target of 90 per cent coverage among girls under 15 by 2030.13
Ireland’s HPV vaccination journey has not been without challenge, but the programme today stands as a testament to public health resilience, evidence-based advocacy, and the enduring impact of one woman’s voice.
Elimination
To assess Ireland’s trajectory toward cervical cancer elimination, CervicalCheck collaborated with Australia’s Daffodil Centre, using national data on HPV prevalence, vaccination uptake, screening coverage, cervical cancer incidence, staging, mortality, and the population prevalence of benign hysterectomy. The modelling confirmed that, with continued high HPV vaccination rates and sustained implementation of HPV-based screening, Ireland is on track to eliminate cervical cancer as a public health problem by 2040 – three years earlier than previously projected.10
Figure 3 illustrates the evolution and success of Ireland’s cervical cancer prevention strategy – from opportunistic screening in the early 2000s to a structured programme incorporating cytology-based screening, HPV vaccination and, more recently, HPV primary screening. The age-standardised incidence rate of cervical cancer peaked in 2009, but has declined steadily since, with further reductions projected as vaccinated cohorts fully transition into the screening programme. This is a remarkable achievement as Ireland is on track to move from having the highest incidence of invasive cervical cancer in Europe in 2009 to being one of the first to reach the elimination threshold by 2040.
Despite this positive trajectory, significant challenges remain. Programme data show that approximately 48 per cent of cervical cancer cases are diagnosed in women who have never been screened, many of whom present at a later stage with poorer outcomes.2 Increasing equitable access and participation is therefore essential to achieving elimination.
To address this, targeted initiatives have been introduced – including age-extension efforts. Between October and November 2023, 107,000 invitation letters were issued to women aged 63-69 for a one-off ‘Exit HPV’ screen. By January 2025, 29 per cent had responded, many of whom had not attended screening in over a decade. This marks an important step in reducing disparities and ensuring that the path to elimination is inclusive, quality-driven, and equitable.
Innovation in equity
The National Cervical Cancer Elimination Plan, launched in November 2024, sets out a clear, equity-driven roadmap to reach under-screened populations through five strategic priorities:
1. Review the introduction of self-sampling to support home-based screening.
2. Conduct feasibility studies on implementation of self-sampling.
3. Reassess triage pathways for HPV-positive results to identify those at higher risk who will most benefit from colposcopy, and additionally attempt to minimise overdiagnosis and overtreatment for women at lower risk.
4. Expand access via community-led initiatives, focusing on:
- Traveller and Roma communities;
- Migrants and refugees;
- People with disabilities;
- LGBTQ+ individuals;
- Women over 50.
5. Deliver a new cervical screening register to improve population tracking and data integration (Ireland’s Cervical Cancer Elimination Plan 2025–2030, p20).
The CervicalCheck programme is examining the evidence on the benefits that self-sampling can add when offered to women who have never been screened or are overdue screening. It is important that a full pathway of care is available for women who test positive on a self-sample as they will then need to attend for a clinician-taken sample to assess if they need colposcopy or not.
As part of the drive toward inclusion, the CervicalCheck Screening Training Unit (STU), in collaboration with the NSS Health Promotion department, is actively working to engage hard-to-reach populations and support non-traditional sampling settings.
These efforts include outreach to Sexual Assault Treatment Units (SATUs), ambulatory gynaecology services, and community-based organisations working with populations experiencing homelessness. The aim is to ensure that cervical screening services are accessible, culturally responsive, and grounded in trusted partnerships.
In parallel, the STU is focused on improving screening uptake among women aged over 50. The STU has developed and delivered tailored education through clinical updates on cervical screening and menopause across multiple platforms – lunchtime learning webinar sessions and recorded clinical updates on our e-learning platform www.nssresources.ie. These are designed to support sample takers in recognising the specific needs of postmenopausal women and tailoring their care accordingly.
Looking ahead, the STU plans to conduct research into the effectiveness of behavioural nudges – specifically, whether sending a text reminder or providing a phone call to women over 50 who are overdue or have not attended screening may increase participation. This work forms part of a broader strategy to reduce inequities and meet WHO elimination targets across all population groups.
This strategic focus reflects WHO’s global guidance on cervical cancer elimination, which places equity at the core – emphasising the need to co-design services with communities and remove structural barriers to participation.
Looking ahead
Ireland’s cervical cancer prevention strategy is dynamic and forward-thinking, and is exploring potential innovations to increase effectiveness, personalisation, and equity. These include:
- HPV genotype surveillance to better understand strain prevalence and population-level risk, informing future vaccination strategy and clinical pathways.
- Revised triage of HPV positive women prior to colposcopy referral, to optimise referral accuracy.
- Risk-based screening intervals, tailored to HPV vaccination status and individual screening history, in line with emerging international evidence.
- Phased implementation of HPV self-sampling, aimed at improving access for under-screened groups, including older women, marginalised populations, and those with practical or psychological barriers to clinician-based testing.
At an international level, Ireland has reactivated its membership in the European Federation for Colposcopy (EFC) and the International Federation for Cervical Pathology and Colposcopy (IFCPC). Ireland is also contributing to global equity efforts, such as screening and colposcopy capacity-building in Ethiopia, where it is supporting training and service delivery in colposcopy and cervical screening.
Conclusion
Ireland’s path toward cervical cancer elimination exemplifies what is possible when evidence, equity, and empathy underpin public health action.
But elimination is not guaranteed. As clinicians, policymakers, and educators, we each have a role in realising this goal. Achieving it will require sustained investment, vigilance, and adaptability in response to population shifts, innovation, and evolving risk factors across the three pillars of vaccination, screening, and treatment.
The strength of Ireland’s strategy lies not only in clinical outcomes, but also in the trust it has rebuilt, the engagement it fosters, and the confidence it instils in individuals to take charge of their health. This is an excellent opportunity for a nationwide commitment from those in the health services in partnership with the general public to work together to make cervical cancer a rare disease in Ireland.
With continued momentum, Ireland is not only on track to eliminate cervical cancer by 2040. We are also on course to lead internationally, setting an example for other countries to follow.
References
- National Cancer Registry Ireland. Cancer in Ireland 1994–2021: Annual Report of the National Cancer Registry. NCRI 2023. Available at: www.ncri.ie
- CervicalCheck Programme Report 2022-2023. Published July 2025. https://assets.hse.ie/media/documents/CervicalCheck_Programme_Report_2022-2023.pdf.
- OECD. EU Country Cancer Profile: Ireland 2025 [Internet]. Paris: OECD Publishing; 2025 Available at: www.oecd.org/health/eucountry-cancer-profile-ireland-2025.htm.
- Minister for Health and Children. Dáil Éireann debate. 29 May 2008. https://www.oireachtas.ie/en/debates/debate/dail/2008-05-29/6/.
- Health Information and Quality Authority. The Role of Human Papillomavirus Vaccines in Reducing the Risk of Cervical Cancer in Ireland. A Health Technology Assessment. February 2008. https://www.hiqa.ie/sites/default/files/2017-02/HTA_HPV_Full_report.pdf.
- CervicalCheck. Programme Report. 1 September 2009 – 31 August 2010. https://assets.hse.ie/media/documents/CervicalCheck_Programme_Report_1_September_2009__2010.pdf.
- World Health Organisation (WHO). Global strategy to accelerate the elimination of cervical cancer as a public health problem. Geneva; 2020. www.who.int/publications/i/item/9789240014107.
- Zarbyn M, Arbyn M, Anttila A, et al. Evidence regarding human papillomavirus testing in secondary prevention of cervical cancer. Vaccine. 2012;30(Suppl 5):F88–F99.
- Rebolj M, Mathews C, Pesola F, et al. The reassuring value of negative HPV tests: A systematic review. BMJ. 2022;376:e068946.
- Simms KT, et al. Projected impact of HPV vaccination and screening on cervical cancer elimination in Ireland. Lancet Public Health. 2024. Forthcoming.
- Pearson J, et al. Trends in cervical screening coverage in England, 2005–2017: Evidence from the NHS Cervical Screening Programme. Public Health England Report. 2020.
- Douglas E, Waller J, Duffy S. Understanding low uptake among young women: Single invitation attendance at age 25 in Greater Manchester. BMJ Open. 2019;9(6):e025360.
- World Health Organisation (WHO). Strategic Advisory Group of Experts (SAGE) on Immunisation: Summary of the April 2022 meeting. Geneva 2022. www.who.int/publications/m/item/summary-ofapril-2022-sage-meeting.
- Dunne S, Coffey L, O’Donnell A, et al. Communicating health risk through personal narrative: The case of HPV vaccine advocate Laura Brennan. Health Commun. 2021;36(10):1286–93.
- Brack J, Brack S, McKenna A. The HPV vaccine controversy in Ireland: An analysis of vaccine hesitancy and public trust. Ir Med J. 2020;113(7).
- Department of Health. Minister for Health announces gender-neutral HPV vaccination from 2019. Available at: www.gov.ie/en/press-release/minister-forhealth-announces-gender-neutral-hpvvaccination-from-2019/.
- Health Service Executive (HSE). HPV vaccine uptake statistics. 2023. Available at: www.hse.ie.