Reference: January 2026 | Issue 1 | Vol 12 | Page 51
Case study
Ella is a 15-year-old girl. She was bullied in primary school for being bigger than her classmates, and was not one of the popular girls. Ella was a little awkward and unsure of herself, and academically always felt behind everyone else. One Christmas, Ella developed migraine and was very unwell for five days, vomiting and bedridden with an excruciating headache.
When she emerged from her five-day indisposition, she noticed her school skirt was a little loose around her waist and her shirt did not gape across her chest. Her mother commented that “she looked like the migraine had done her a favour”, and that in fact, she herself “wouldn’t mind one” if it meant she would lose a pound or two.
Ella experienced a feeling that was alien to her but wonderful. She felt a thrill of self-esteem, a sense of excitement, and something that later she could only describe as “power”. From this moment on, Ella pursued this feeling. Initially, she decided to cut back on deserts and biscuits after her dinner. She had tried to do this in the past, but had never managed to get beyond supper time.
This time it was different – she had been gifted the sweet experience of weight loss before the self-denial, and this was more motivating than any imagined feeling of weight loss. Sickness had given her the cart before the horse and she was determined to maintain this feeling.
After less than a month, a few girls at school and her PE teacher commented on her new svelte appearance, and Ella finally felt like she had something she was good at. Girls who in the past did not acknowledge her existence were suddenly asking her what diet she was following and were interested in what she had to say. Ella felt like she mattered, that she belonged, and that she now had a kind of currency that bought her a place with her peers. She was no longer on the verges – a loser looking in.
Ella goes on to lose more weight. She gave up all sweets, chocolate, ice cream, milk in her tea, etc, for lent that year and joined the local athletics club. There she discovered a gift for long-distance running and became part of the club’s team. She had really found her place socially and the overweight, awkward little girl became a distant memory.
It was the following Christmas when things took a sinister turn for Ella. She had started to skip meals in September when she went back to school, managing without a breakfast and eating only fruit for lunch because she was training at lunch-time.
By December she was feeling weak, cold all the time, and irritable. For reasons that she could not explain, on Christmas evening, when everyone was sitting down watching a film and she was in the kitchen making a black coffee, she, almost in a trance, took a spoonful of trifle, that led to another and another. She described it as “someone else took over my body”.
“It was like another part of myself was screaming STOP in my head. I suddenly came back to my senses and was in a panic. My iron will was suddenly gone.”
Ella went to the bathroom, locked the door, and put her fingers down her throat for the first time. The food came back up easily, including the small amount of turkey and vegetables she had eaten earlier. Ella said it was as though she had discovered a “secret weapon”.
“Looking back now, I wish I had never done that,” she said. “No, looking back, I wish someone had told me when I was 15 and struggling to find my place in the world, that it was normal to feel that way, and that all teenagers feel like they don’t fit in or belong.”
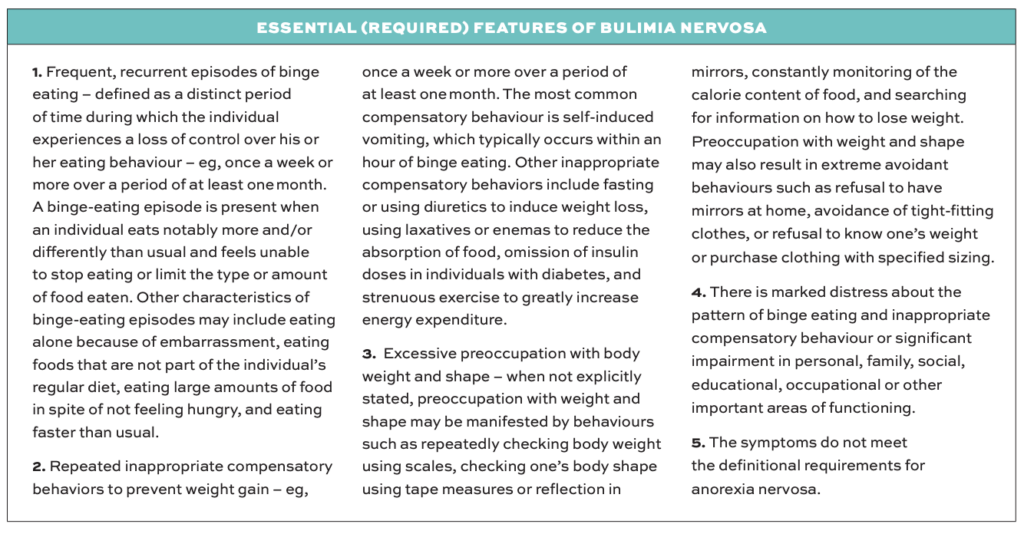
Recognising bulimia
When you meet somebody like Ella in your daily practice, you might see someone who can range from underweight to normal, or a little overweight, as purging does not rid the body of all the calories ingested in a binge. As the bulimia progresses, the binges get bigger and a person can take in up to 3,000 calories in one sitting. Around 40 per cent of these calories are absorbed despite vomiting.2
Therefore, you may not suspect an eating disorder in the first instance. Many of our patients report staff making comments like “you’re not that thin” or “you look a healthy enough weight”. These kinds of comments often cause shame for many sufferers, and a perception that they are not sick enough to get help, and individuals may not attempt to access support again for some years.3 This leads to poor long-term outcomes and greater risk of comorbidities.4
Clues you may be dealing with bulimia nervosa may include swollen parotid glands, giving the cheeks a slightly swollen appearance. There may be callouses on the fingers from purging (Russell’s sign), though many individuals either use a toothbrush or can voluntarily purge using their diaphragm muscles. The individual may complain of frequent dental issues, abdominal pain, bloating, amenorrhoea, diarrhoea, or constipation.
Blood tests may show deranged electrolytes, especially potassium, which is depleted by laxative abuse and purging. However, many blood results and vital signs are within normal parameters. Commonly reported complications of bulimia nervosa are illustrated in Table 2.
It is important to note that this list is not exhaustive, and gives only a guide to some of the medical presentations that might raise the index of suspicion that you are seeing a presentation of bulimia nervosa. For a more comprehensive and in-depth guide to potential medical risk and complications, and management of same, please refer to resources such as Medical Emergencies in Eating Disorders: Guidance on Recognition and Management and Medical Management of Eating Disorders.7,8
Tip: Advise individuals who are purging frequently not to brush their teeth after vomiting as this coats the teeth in stomach acid, causing significant damage to the teeth. Recommend that they swirl the mouth with water and eat some sugar-free gum.
Conclusion
Patients with eating disorders often experience judgement, stigma, and dismissal during their interactions with healthcare staff, which often delays or prevents help-seeking behaviours.9,10
It is understandable that healthcare professionals, who may not fully understand the predisposing, precipitating, and perpetuating factors that form the foundation and maintenance of eating disorders, might think that this individual in front of them with a body mass index of 16kg/m2, a serum potassium level of 1.9mmol/L, and an ambivalent, possibly resistant, attitude toward treatment, is somehow to blame for their illness. Some staff may even think it is self-inflicted, attention seeking, and just a little bit vain. However, the reality is somewhat different.
I ask you to remember that Ella– the girl in front of you – who you might think is being a little bit challenging and irresponsible – is, in reality, protecting her special feeling of belonging, of being able to stand with pride among her peers, and of finally being seen. She desperately fears going back to being the overweight, awkward girl watching life from the verges, with no friends.
When we dig a little deeper into Ella’s life, we find a mum who has a subclinical eating disorder and suffers from untreated anxiety. From Ella’s description, it sounds as though her mother had suffered postnatal depression following the birth of Ella and her younger brother. Ella’s father is an alcoholic and abusive when intoxicated.
Ella’s eating disorder was most likely predisposed by her genetics, childhood trauma, and bullying at school – all of which are recognised factors that load the gun for an eating disorder.
The migraine-induced weight loss pulled the trigger and the sudden feelings of agency, belonging, and self-soothing in the context of profound low self-worth, added to by the preoccupation with weight and food that is the hallmark of eating disorders, maintained her bulimia. For Ella, bulimia was not a choice but a solution. We cannot hope to support her recovery without understanding what brought bulimia into her life and helping her find alternative solutions. This is the work.
| BODY SYSTEM | MEDICAL COMPLICATION |
|---|---|
| Skin | ▶ Callous formation on dorsal aspect of the hand (Russell’s sign) ▶ Xerosis (dry skin) ▶ Alopecia |
| Eyes, ears, and nose |
▶ Sub-conjunctival haemorrhage from self-induced vomiting ▶ Epistaxis |
| Dental | ▶ Dental erosion, periodontal disease, hypersensitive teeth ▶ Sialadenosis (inflammation of salivary glands giving bilateral swelling) ▶ Raised amylase in 61 per cent of bulimia patients who purge (from salivary glands, not pancreas)6 |
| Throat | ▶ Vomiting-induced acid reflux can damage oesophageal sphincters, pharynx, and larynx (laryngopharyngeal reflux) ▶ Acid contents may impact vocal cords causing hoarseness, cough, dysphagia, or repeated sore throats |
| Gastrointestinal | ▶ Gastro-oesophageal reflux, painful swallow (odynophagia), oesophagitis, oesophageal erosion with/ without ulcers and bleeding (all from repeated exposure to stomach acid) ▶ Barrett’s oesophagus and increased risk of oesophageal cancer ▶ Boerhaave’s syndrome (oesophageal rupture), although rare, is a serious medical/surgical emergency ▶ Laxative abuse can cause significant functional impairment in the colon including loss of colonic peristalsis from habituation. Stimulant laxatives can have a toxic effect on the colon and can cause irreversible damage (colostomy, incontinence) |
| Electrolytes | ▶ Low serum potassium from purging, laxative and/or diuretic misuse, or renal loss due to exchange for sodium to prevent volume depletion ▶ Low total body magnesium can increase urine loss of potassium about 30 per cent of the time7 |
| Cardiac | ▶ Hypokalaemia can prolong the QTc interval, increasing risk of arrhythmias which may lead to syncope, palpitations, and torsades de pointes |
| Pulmonary | ▶ Risk of aspiration from self-induced vomiting ▶ Pneumomediastinum (air between the two lungs caused by retching) ▶ Occasionally, foreign objects like spoons and toothbrushes have been found in the oesophagus, lung, and stomach from accidental ingestion |
TABLE 2: Possible complications of bulimia nervosa5
References
- World Health Organization. International statistical classification of diseases and related health problems (11th Edition). Available at: www.icd.who.int/en/.
- Kaye WH, Weltzin TE, Hsu LK, et al. Amount of calories retained after binge eating and vomiting. Am J Psychiatry. 1993 Jun;150(6):969-71. doi: 10.1176/ajp.150.6.969.
- Wall PL, Fassnacht DB, Fabry E, et al. Understanding stigma in the context of help-seeking for eating disorders. J Eat Disord. 2024 Sep 2;12(1):126. doi: 10.1186/s40337-024-01086-w.
- Treasure J, Claudino AM, Zucker N. Eating disorders. Lancet. 2010 Feb 13;375(9714):583-93. doi: 10.1016/S0140-6736(09)61748-7.
- Mehler PS, Rylander M. Bulimia Nervosa – medical complications. J Eat Disord. 2015 Apr 3;3:12. doi: 10.1186/s40337-015-0044-4.
- Kinzl J, Biebl W, Herold M. Significance of vomiting for hyperamylasaemia and sialadenosis in patients with eating disorders. Int J Eat Disord. 1993 Jan;13(1):117-24. doi: 10.1002/1098-108x(199301)13:1<117::aid-eat2260130114>3.0.co;2-8.
- Birmingham CL, Treasure J. Medical Management of Eating Disorders, 3rd Edition. Cambridge Press: UK.
- Royal College of Psychiatrists. Medical emergencies in eating disorders. 2022. Available at: www.rcpsych.ac.uk/improving-care/campaigning-for-better-mental-health-policy/college-reports/2022-college-reports/cr233.
- McNicholas F, O’Connor C, O’Hara L, McNamara N. Stigma and treatment of eating disorders in Ireland: Healthcare professionals’ knowledge and attitudes. Ir J Psychol Med. 2016 Mar;33(1):21-31. doi: 10.1017/ipm.2015.24.
- O’Connor C, McNamara N, O’Hara L, et al. How do people with eating disorders experience the stigma associated with their condition? A mixed-methods systematic review. J Ment Health. 2021 Aug;30(4):454-469. doi: 10.1080/09638237.2019.1685081.
