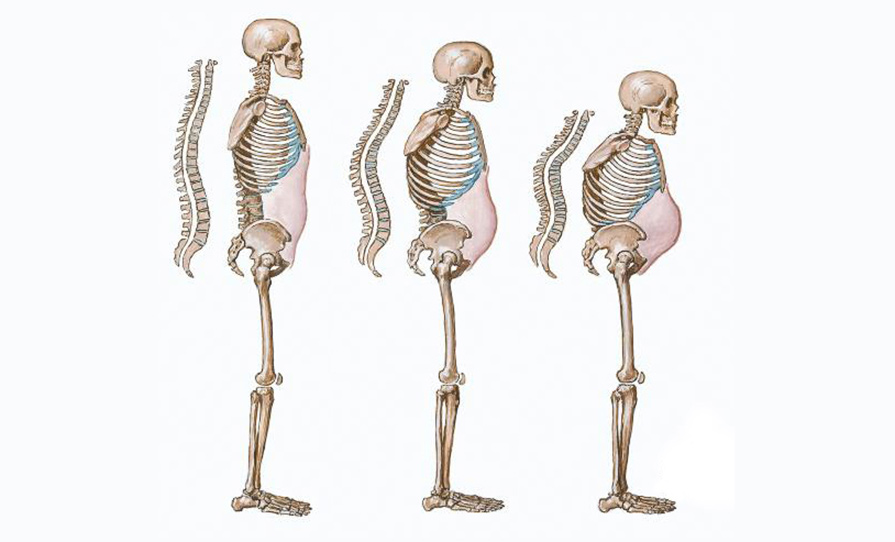
A recent study has found that bone fracture protection fades within a year of stopping hormone replacement therapy (HRT).
In the study, published in Lancet Healthy Longevity, experts from the School of Medicine at the University of Nottingham also found that, in most cases, stopping treatment is then followed by some years of elevated fracture risk compared to women who have never used HRT. Fracture risk then falls to be similar to, and then lower than, women who have never used HRT. The researchers used data from six million women collected at around 2,000 GP surgeries in the UK, which allowed them to follow up fracture risk levels for up to 25 years.
Lead author Dr Yana Vinogradova, Centre for Academic Primary Care in the School of Medicine, University of Nottingham, said: “The findings of our study confirmed that women on menopausal hormone therapy (MHT) show a progressively reducing fracture risk compared with women not using MHT. More importantly, we also observed a clear pattern of risk change after therapy was discontinued.
“For most women, the bone protective effect of MHT use disappears completely within about one year of treatment being stopped, then their fracture risk rises compared to never users, peaking after about three years, before declining to become again equivalent to never users – about 10 years after discontinuation – and then again continuing to decline relative to never users. So, even after stopping MHT, women should benefit from notably reduced fracture risk in their later decades.”
This observed risk pattern was the same for all menopausal hormonal treatments, but the level of excess risk depended on the treatment type and the length of past MHT use.
“Our comparative illustration of observed patterns of fracture risk for short and long use can help doctors and patients when discussing MHT treatment options, and to consider how fracture risk may change after stopping MHT use.
“Anticipating periods of increased risk might prompt doctors to check patients’ bone health at discontinuation, particularly for patients most at risk with other fracture risk factors such as smoking or inactivity. These novel findings may also usefully stimulate further clinical and biological research into these treatments,” added Dr Vinogradova.