In her series on Irish figures who have left their mark on medical history, Bette Browne looks at the career of Nobel Laureate Prof William Campbell, who developed a treatment against river blindness
Irishman Prof William C Campbell revolutionised the treatment of some of the world’s most devastating parasitic diseases and turned lives of inevitable darkness into light for millions of people when he developed a treatment against river blindness, a breakthrough that won him the 2015 Nobel Prize in Medicine.
Fortunately for the medical world, worms always fascinated Prof Campbell. “My interest in biology was always about parasites, parasites of all kinds, especially parasitic worms,” he once said.
“I consider them beautiful. They’re just doing their own thing. I have said that the objective is not to get rid of parasitic worms; the objective is to get rid of parasitic diseases.”

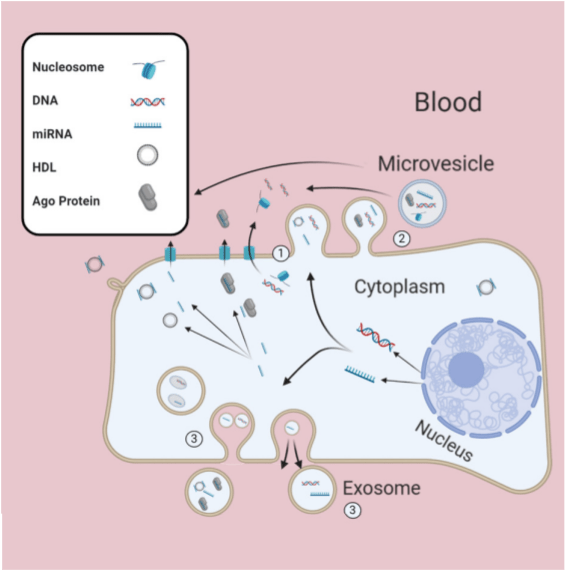
Prof Campbell’s study of worms “doing their own thing” would ultimately lead the biologist and parasitologist to discover a breakthrough therapy using derivatives of avermectin to fight parasitic diseases and infections caused by roundworms that plague over half of the world’s population.
The Campbell regimen is simple: A single tablet taken once a year over the course of 16-to-18 years, since it kills only the worms’ larvae, and it can take up to 18 years for all the adult worms in a body to die. It cannot restore lost sight, but a course of the medication will halt the progression of the disease, so blindness is no longer inevitable.
Before Prof Campbell’s discovery of the drug, the only real weapon against river blindness was an insecticide sprayed over the fast-flowing rivers and streams in which blackflies breed. While such spraying helped reduce blackfly populations, it never came close to eliminating the disease.
Prof Campbell, in a proud moment for Ireland in 2015, shared half of the Nobel Prize for Physiology and Medicine with his Japanese colleague, microbiologist Prof Satoshi Omura, for their joint research, the other half of the prize going to Chinese scientist Youyou Tu for her discovery of a therapy against malaria.
Breakthrough
Forty years earlier, in the late 1970s, while working at Merck Research Laboratories in the US with a batch of microbe strains that Omura had sent from Japan for evaluation, Prof Campbell developed a drug using ivermectin, derived from avermectin, believing it would work for river blindness in humans. Not only did the drug work, it also proved effective against the parasite that causes elephantiasis, which results in severely swollen limbs in seriously affected cases and can coexist with river blindness. It was a momentous breakthrough.
“Diseases caused by parasites have plagued humankind for millennia and constitute a major global health problem,” the Nobel Assembly at Karolinska Institute said when it decided to award the 2015 Nobel Prize to Prof Campbell and his colleague. “In particular, parasitic diseases affect the world’s poorest populations and represent a huge barrier to improving human health and wellbeing. This year’s Nobel Laureates have developed therapies that have revolutionised the treatment of some of the most devastating parasitic diseases.
“William C Campbell and Satoshi Omura discovered a new drug, avermectin, the derivatives of which have radically lowered the incidence of river blindness and lymphatic filariasis, as well as showing efficacy against an expanding number of other parasitic diseases. Youyou Tu discovered artemisinin, a drug that has significantly reduced the mortality rates for patients suffering from malaria.
“These two discoveries have provided humankind with powerful new means to combat these debilitating diseases that affect hundreds of millions of people annually. The consequences in terms of improved human health and reduced suffering are immeasurable.”
It was high praise for Prof Campbell’s pioneering work, which has since transformed the lives of millions of people around the world, especially in poorer regions. Most infections occur in sub-Saharan Africa, although cases have also been reported in Yemen and parts of Central and South America.
River blindness, or onchocerciasis, is caused by a tiny worm that can infect the cornea and cause blindness. Lymphatic filariasis, or elephantiasis, is also caused by a worm and produces chronic swelling.
Today, thanks to Prof Campbell’s breakthrough decades ago, the World Health Organisation (WHO) has moved from treating river blindness to eliminating it.
In 2017, for example, more than 145 million people were treated in Africa, where the community-directed treatment with ivermectin (CDTI) programme was implemented. This compared with 46 million in 2005 and represents more than 70 per cent coverage of the number of people who require treatment globally.
Since 2009, the WHO’s focus on river blindness has shifted from treatment to elimination, and today four countries have been verified by WHO as free of onchocerciasis — Colombia, Ecuador, Mexico, and Guatemala.
Background
William Cecil Campbell was born in Derry on 28 June 1930, and grew up in Ramelton, Co Donegal. It was there that his fascination with worms began. “Ramelton was the place where I first became aware of the existence of parasitic worms and medicines to get rid of them in animals,” he recalled.
His father farmed in Donegal, raising shorthorn dairy cattle that won prizes at agricultural shows and it was at one such show that 14-year-old Campbell picked up a pamphlet on how to rid livestock of worms. It sparked a fascination with the subject and is said to have influenced his decision to become a scientist.
He studied in Belfast and at Trinity College Dublin (TCD), from which he received a BA in 1952. TCD, and specifically Prof JD Smyth, had a major impact in shaping his career, as Prof Campbell recalled in his Nobel lecture in 2015.
“(In TCD) I came under the influence of Dr JD Smyth, who was making a name for himself in the field of invertebrate physiology and especially in the area of experimental parasitology. He became (informally, of course) my mentor, and he changed my life. Among the things that Prof Smith did for me as I approached graduation was to respond positively to enquiries from Prof Arlie Todd of the University of Wisconsin, US. The result of that communication was my application for graduate school at the University of Wisconsin, along with two other Trinity students. Both of the others dropped out, and before I set out on that journey alone, one of them sent me a note saying: ‘For God’s sake, don’t panic when you get off the boat.’”
He didn’t panic, but instead knuckled-down and received a doctorate at the University of Wisconsin-Madison in 1957. From 1957 to 1990, at the Merck Institute for Therapeutic Research in New Jersey, he was involved in the development of ivermectin.
In his Nobel lecture, ‘A Reflection on Simplicity’, Prof Campbell recalled starting the research on 9 May, 1975, when a single mouse in a mouse-box was infected with parasitic worms — not enough to cause illness — and then fed a special food to which a fermented substance had been added. The results would spark ground-breaking medical advances.
“On that day (9 May), its diet was altered — some liquid was stirred into its regular food and the mouse ate that food for almost a week. Then its normal diet was restored. And about a week after that, its worms had gone. From that moment, a train of events was set in motion. It would lead, some years later, to an advance in medical and veterinary science, and that, in turn, would lead to practical changes in the management of parasitic disease. To a very large extent, the drug ivermectin was brought about by simple science.”
Then began years of complex research. “Simplicity, in the history of ivermectin, was just a beginning. From then on, there was complexity — years of complex basic research and years of complex developmental research. Pharmaceutical development is the epitome, not of simplicity, but of complexity.”
In 1978, having identified a successful treatment for a type of worms affecting horses, Prof Campbell realised that similar treatments might be useful against related types of worms that affect humans. In 1981, Merck carried out successful phase 1 treatment trials in Senegal and France on river blindness and went on to study the treatment of elephantiasis.
In 1987, nine years after Prof Campbell first floated the idea, Merck Research Laboratories announced it would distribute the drug ivermectin free wherever it was needed. In Prof Campbell’s words, the gesture has helped to combat “forgotten diseases of forgotten peoples”. To date, according to the company, more than one billion treatments have been donated to some 117,000 communities in Africa, Latin America and Yemen.
But the free distribution of the drug was more than an altruistic gesture, Prof Campbell suggested after winning his Nobel, because in an inter-dependent world, it is incumbent on those in the developed world to treat diseases wherever they occur.
Prof Campbell has also urged scientists to look beyond the “glamour of high science” and instead look back to nature in their search for drugs. “One of the big mistakes we’ve made all along is that there is a certain amount of hubris in human thinking that we can create molecules as well as nature can,” he said.
“I have recently made a proposal to search the earth more broadly for new natural products as a means of finding novel molecules for chemotherapeutic development. The focus would be primarily on substances produced in microbial fermentation, but could be broadened to include substances made by other forms of life. The target utility of screening new substances would not necessarily be limited to the field of infectious diseases, or even to medicine at all. I have, on occasion, called it my ‘unpopular proposal’ — unpopular because it is destitute of the glamour of high science but though it harkens back, it also looks forward. It would not rely only on science — it would depend, crucially, on the talent abundantly available in the realms of logistics, finance and management.”
In 2002, Prof Campbell was elected member of the US National Academy of Sciences. But one of his most treasured accolades came in December 2017, when President Michael D Higgins awarded him a Presidential Distinguished Service Award for the Irish abroad.
More recently, on 20 May 2019, the Department of Education established a third-level scholarship to honour Prof Campbell. Minister Joe McHugh said the aim of the award was to encourage the next generation of Irish students to strive to replicate achievements like Prof Campbell’s, which have transformed the lives of millions of people across the world.
From 1990 to 2010, when he retired, Prof Campbell was a research fellow at Drew University in Madison, New Jersey. He was well known there, not only as a Nobel Laureate, but also an accomplished poet and painter, whose works reflect his life-long fascination with parasitic worms.
Sources: Nobel Prize committee, Irish America, WHO, Drew University, New Jersey Monthly, The Lancet.











Leave a Reply
You must be logged in to post a comment.