DR SILE KELLY1, SpR in Public Health; and DR BREDA COSGROVE1, Specialist in Public Health Medicine. 1Department of Public Health Mid-West, Limerick
Food is important in so many aspects of life and health. It can bring joy, love, comfort, cultural expression, and good health. But like many will know there is a dark side to food, in particular when it is inadequate, in excess, contaminated, or of poor quality. Food is powerful. Food and food choices can carry and increase the risk of diseases, result in malnutrition, contribute to climate destabilisation and even cause death. Trying to address these health issues can sometimes feel as helpless as facing an asteroid hurtling towards Earth. The impact of food-related disease can have a significant impact on an individual’s health, but also cause a chain-reaction that is felt across healthcare and society for many years to come. This article will review the public health consideration of food and nutrition, and the important interventions that physicians can integrate into their daily practice, benefitting patients and the wider population.
Food and disease
Communicable and non-communicable disease can arise from food and malnutrition. This is something that physicians encounter on a daily basis, through their management of people with obesity, cardiovascular disease, infectious colitis or gastroenteritis, and many more conditions.
Food and infectious disease
(i) H. pylori
The bacteria helicobacter pylori (H. pylori) can infect the stomach and cause a spectrum of symptoms and disease. It not only affects the infected individual, but also has wider healthcare implications. H. pylori is thought to be transmitted through contaminated food and water, as well as person-to-person spread. It can be carried asymptomatically, cause gastritis, ulcer formation, gastric adenocarcinoma and MALT lymphoma, as well as contribute to the burden of dyspepsia in the population. It has been estimated that approximately 40 per cent of the population will at some time in their lives experience dyspepsia, and 2 per cent will lose time from work because of it. Approximately 20-to-50 per cent of populations in Western countries are infected with H. pylori, and up to 80 per cent of populations in developing countries. Of these, 10 per cent will develop a duodenal or gastric ulcer, and up to 3 per cent may develop gastric cancer and MALT lymphoma. H. pylori is therefore an important health problem, and a significant contributor to the global burden of disease.
A ‘test and treat’ strategy has been shown to be effective in eradicating H. pylori. It also significantly reduces the need for endoscopy by approximately two-thirds of cases. This contributes to an overall reduction in healthcare costs. The annual national cost of elective day case upper gastrointestinal (GI) endoscopy performed in Ireland is an estimated €29.9 million per year.
To maximise health and healthcare benefits, H. pylori should be eradicated. This in turn should be confirmed with follow-up investigations to ensure eradication has been successful. Eradication of H. pylori is the most effective way in preventing the recurrence of duodenal ulcer, and contributes to the reduction of the burden of dyspepsia and other negative outcomes of H. pylori infection (see Table 1). Population screening for H. pylori bacteria in the Irish context has previously been discussed. There are potential positives of screening, however, there are additional considerations such as antimicrobial stewardship, and demand on services. This is a particular consideration with increasing antimicrobial resistance as well as the pandemic having given rise to a backlog of healthcare delivery. An effective local implementation of a ‘test and treat’ strategy, with follow-up for eradication, has the potential to significantly decrease the burden of disease in our populations, decrease the use of long-term medications, and reduce the burden on endoscopy departments.
| OUTCOME | NNT | SOURCE |
| Recurrence of duodenal ulcer at 12 months | 2 | Delaney, 2006 |
| Eradication of functional dyspepsia | 15 | Delaney, 2006 |
| Reduction of incidence of gastric cancer | 124 | Ford et al, 2020 |
Table 1: Estimated number needed to treat (NNT) for H. pylori eradication that results in a positive health outcome
(ii) Food poisoning
Another common communicable disease encountered in gastroenterology is ‘food poisoning’; gastroenteritis and infectious colitis. Verocytotoxigenic E. Coli (VTEC) is a particular issue in Ireland (see Figure 1), and a significant public health burden. VTEC can be spread from person-to-person, through contact with farm animals or through contaminated food and water. Ireland has the highest incidence of VTEC in Europe at a rate of 18.6/100,000. Once again, its impact is not only a risk to the infected individual, but additionally causes major challenges to close contacts and the healthcare setting.
There is a risk of developing haemolytic uraemic syndrome (HUS) in 5-to-12.5 per cent of people with VTEC, in particular in paediatrics and the elderly, which can be fatal in 3-to-5 per cent of people. Approximately 12 per cent can have long-term sequelae from HUS. VTEC can be suspected not only on clinical grounds based on symptoms, but also on epidemiological grounds, such as contact with farm animals or using drinking water from an untreated private well. It has a low infectious dose, can be carried asymptomatically, and have prolonged shedding of the virus in stool.
In a healthcare setting, there are a number of vulnerable persons at higher risk of acquiring and spreading the infection. Healthcare workers play an important role in reducing that risk through good hand washing and food handling practices. A healthcare worker who contracts VTEC will also be required to submit two negative stool samples in order to return to work (ie, microbiological clearance). In adults, VTEC can take on average seven days due to viral shedding, and in children it could take several weeks following the resolution of diarrhoea. Antibiotics are ineffective in treating VTEC. Prevention is better than cure, and therefore handwashing is better than repeated stool samples.
Food and nutrition
There are also many non-communicable diseases associated with food and nutrition that have a wider public health impact. The healthcare system in Ireland faces the double burden of malnutrition that includes undernutrition as well as obesity.
(i) Undernutrition
Malnutrition is a significant health issue in Irish hospitals. One-in-three people admitted to hospital is malnourished. Undernutrition can increase a person’s risk of infection, pressure sores, falls, readmission, and death. There is also an associated increased healthcare cost and prolonged hospital stays in those who are malnourished. Overall it results in poorer outcomes for patients, with many of these potentially avoidable. Disease-related malnutrition annual costs are estimated to be €1.42 billion, representing more than 10 per cent of the total health and social care budget. Screening at-risk patients with a validated screening tool will result in early detection and management of those at risk. Widespread implementation of screening for malnutrition such as the Malnutrition Universal Screening Tool (MUST) at admission will result in more effective interventions, improve patient outcomes and reduce healthcare costs. Trainees can avail of nutrition study days, a core part of higher specialist training (HST), to support their education and deepen their understanding of their role in the prevention of malnutrition-related health outcomes.
(ii) Obesity
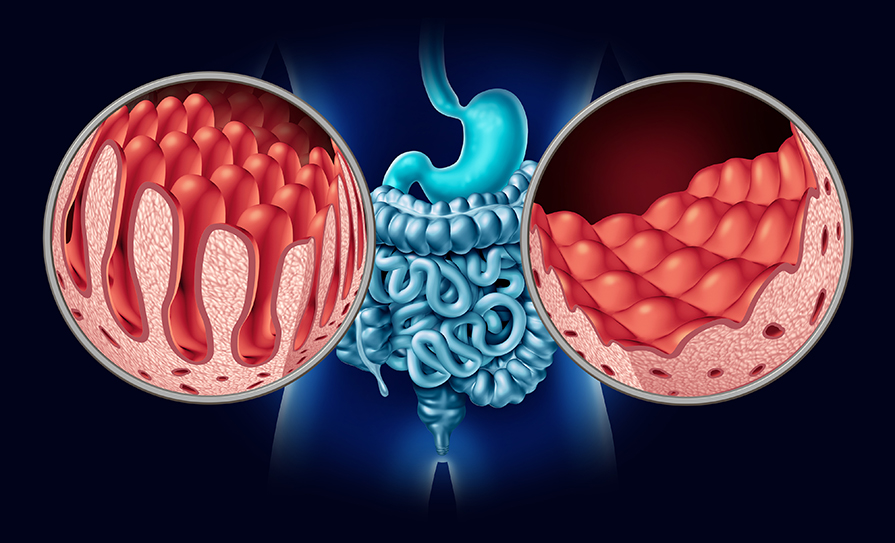
On the other end of the spectrum is obesity. Ireland has one of the highest levels of obesity in Europe with 60 per cent of adults and more than 20 per cent of children living with overweight and obesity. Obesity increases the risk of developing a number of GI health issues, including but not limited to Barrett’s oesophagus, gastroesophageal reflux disease (GORD), inflammatory bowel disease (IBD), colonic polyps, and some GI cancers such as oesophageal, gastric, colorectal, hepatocellular, and pancreatic cancer. The endoscopic investigation and management of these conditions is further complicated by obesity. Some studies have shown that people with obesity may require more aggressive bowel prep, and there is speculation that there may be increased difficul
ty achieving caecal intubation, potentially prolonging the procedure, increasing the risk to the patient, and the risk of an incomplete procedure. Gastroenterology clinics and endoscopy are seeing a rise in patients living with obesity.
Figure 1: VTEC cases in Ireland between 2015-2020 adapted from the HPSC website*. *2018 and 2019 are estimate figures only.
Screening and brief health interventions for obesity can be effective in supporting weight loss. In clinical practice, it is rare to make these opportunistic interventions on weight. Healthcare workers are among the most trusted in society as an information source, and screening opportunistically and advising on weight loss can help support your patients to improve health. This can be further enhanced by supporting them through referral to an available community weight-loss programme. This may cost the health service initially, but one study in the UK showed that a community weight-loss programme is cost-effective from the third year and cost-saving from the ninth year onwards over an entire 20-year period, as it reduces the number of obesity-related health conditions. Ireland currently has some community weight-loss programmes on offer that may be available in your catchment area.
(iii) Adequate nutrition
Adequate nutrition is one of the most effective (and least costly) ways to decrease the global burden of disease. Screening for malnutrition and early involvement of dietetics are important tools at a physician’s disposal. Moreover, to further support adequate nutrition, the HSE has a ‘Healthy Food for Life’ campaign with many readily available online resources. They have healthy eating guidelines for all people over the age of five years, including for older and pregnant or breastfeeding people. The 101 Square Meals recipe book is a freely available starting point for those people that are open to improving their nutrition.
Understanding and supporting nutrition is an important part of the national Gastroenterology and Hepatology Higher Specialist Training (HST) curriculum: “To understand energy homeostasis, under nutrition and be capable of determining nutritional status, applying that knowledge and appropriate skills to providing additional nutritional support….”
Despite the importance of nutrition as a leading cause of morbidity and mortality, nutrition being a recognised learning outcome in HST, and patients placing their trust in doctors as their information source on nutrition, many physicians are not confident in their nutrition-related counselling skills. This represents a gap in the needs of our patients and the delivery of care. To mitigate against the rising tide of nutrition-related illness, doctors should be skilled in meeting the needs of the people they serve and empower people to achieve better health outcomes. The Irish Society for Clinical Nutrition and Metabolism (IrSPEN) has a number of educational and professional resources, including the Life Long Learning (LLL) Programme for medical professionals.
Food and climate
Healthcare is a major contributor to climate destabilisation, and therefore paradoxically a contributor to the burden of disease in our patients. Food, including hospital food, has an important role in its intersectional and pivotal place in climate destabilisation. Globally, Ireland is considered a ‘major emitter’ of greenhouse gases which contribute to climate breakdown, and is considered one of the worst in the European Union. An estimated 71 per cent of emissions from healthcare are derived from the healthcare supply chain; the goods and services an organisation avails of. These are known as scope 3 emissions. They are as of a result of the activities of healthcare but are not owned or controlled by the institution itself, eg, pharmaceuticals, medical devices, personal protective equipment (PPE). Of these, 9 per cent are associated with the provision of food and agricultural products. It is estimated that up to 49 per cent of the food provided to patients in Irish hospitals is not eaten. Uneaten food is wasted food, is not contributing to nutrition, but directly contributing to increased costs and increased emissions. Early consultation with dietetics to tailor the food to the nutritional needs of the patient can reduce food waste, reduce the climate impact, and support your patients’ health.
Conclusion
NASA and the European Space Agency (ESA) are currently involved in a mission that aims to nudge an asteroid off course and away from Earth. The asteroid causing concern is 11 million light years from Earth, and is not an immediate threat, but they are preparing now. Much like an asteroid, being conscious of the role food and nutrition plays in the health of our patients and implementing strategies to redirect their course toward better health outcomes is preventative. Food and nutrition play a powerful and complex role in health and healthcare in Ireland, and healthcare workers are an important driver in the direction of their patients’ health. Incorporating preventive practices on a daily basis for the future health of patients, wider society and the planet, can feel like nudging an asteroid that is impossibly far away. It takes awareness, extra time, uncertainty if it will work every time, and the results will take years to see. Unlike deflecting an asteroid, we have clear evidence that adequate nutrition is an effective and low cost way to reduce the global burden of disease. Taking the time in daily practice to screen for food-related infectious diseases, to screen for malnutrition on admission, to screen people living with obesity who may be ready and accepting of change, and to further our education in nutrition counselling may just nudge the trajectory of your patients’ health out of the path of disease.
References on request










Leave a Reply
You must be logged in to post a comment.