Paul Mulholland examines recent HSE documents regarding its monitoring of the private activity carried out by consultants
In April 2018, the Department of Health requested that the HSE establish a framework to ensure compliance with the terms of the consultant contract regarding private practice. The Department requested that the HSE’s Internal Audit Division be consulted on the establishment of the framework and that consultant compliance form part of the Executive’s annual internal controls process. It was also requested that the HSE’s audit committee be asked to include consultant contract compliance in its work programme.
The request was made shortly before the High Court settlement in June 2018 on monies owed under the consultant contract. The Department and HSE lost the case. The estimated cost of the settlement was €182 million for arrears and ongoing costs of €62 million per annum from 2019, backdated to the date of the settlement. Before 2014, compliance with the contract had national oversight. However, in 2014 this was delegated to the Hospital Group CEOs. Monthly reporting by individual hospitals to the National Director of Acute Hospitals was no longer a requirement. The new
framework was created to re-introduce oversight at a national level.
Through Freedom of Information legislation, the Medical Independent has obtained the 2019 annual report on the private practice of public hospital consultants and their adherence to private practice limits set in the consultant contract. The report, which was completed in August of last year, stated that a number of issues highlighted in the 2018 report had been addressed “in order to enable effective oversight”.
The 2018 report noted there were challenges in assessing compliance for consultants who were contracted in multiple sites because the ‘paymaster hospital’ was required to oversee compliance, but did not have access to the data for the other sites. Due to complexities relating to data-sharing, hospitals have now been instructed to report their own activity only, regardless of consultant discharges in other public hospitals.
“Subsequently, if a consultant in a hospital, who holds a split appointment over two or more hospital locations, reports a high ratio of private activity in one location his/her activity should then be reviewed in the context of services provided by the consultant over all sites by combining the weighted units,” according to the 2019 report.
Treatment of locum consultants, in assessing overall compliance, was an open item at the time of the previous report. Since then, it has been agreed that locum consultants should be included in the process in the same way as consultants on contracts. Completeness of hospital inpatient enquiry (HIPE) coding within 30 days on a number of sites was a challenge for many hospitals. This resulted in delayed reporting and amended data.
“This has been addressed with the Hospital Groups by improvements to the report templates generated by the Healthcare Pricing Office (HPO) and through training and communication with the hospitals,” according to the 2019 report. The report stated HR/medical administration capability remained a challenge.
“However, familiarity with the reporting requirements and the data has meant greater levels of reporting compliance,” it stated. The 2019 report said mechanisms are still required to include outpatient and diagnostic activity so that overall compliance can be measured more effectively. No effective mechanism has been identified to date.
“The expansion of the ABF [activity-based funding] model and the use of NIMIS [National Integrated Medical Imaging System] may offer opportunities to address this issue and this is being examined by Acute Operations in consultation with CIO [Chief Information Officer] and HPO.”
Public/private mix
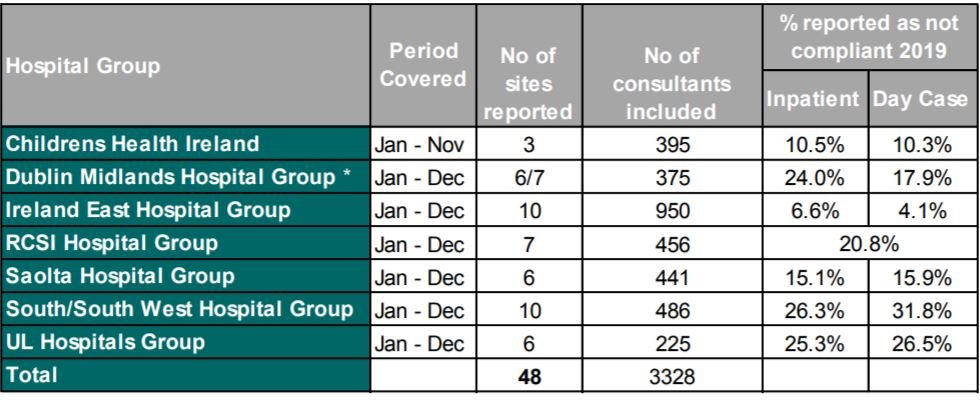
According to the 2019 report, 13.9 per cent of patients seen by public hospital consultants were on a private basis. This was below the 20 per cent threshold set in the contract and is evidence of a “general adherence to limits” (see Table A for a breakdown per Hospital Group). In 2018, the percentage was 15.4 per cent. A review of non-compliance with public/private mix has highlighted a number of factors which are largely outside of the control of the hospitals or consultants, and can contribute to overall levels of public/private activity. Foremost among these is emergency admissions.
“Emergency admissions account for most of the inpatient workload. In these cases the consultant on call is assigned the patient irrespective of the patient insurance status and therefore it is outside of the consultant’s control,” according to the report.
“To put this into context, 69 per cent of all inpatient discharges in 2019 were admitted on an emergency basis (2018 – 68 per cent).”
Other factors include: The specialist services that the hospital provides; whether it is a larger hospital providing emergency and complex care or it is a smaller hospital with less complex emergency, day case and elective care; whether comparable services are available in a near-by private hospital; where there is no private hospital located in the same region as the public hospital all required private work will be carried out in the public hospital; and the various consultant contract types within the hospital.
The report also noted if consultants in the hospital hold split appointments in that they work over two or more hospital locations – a high ratio of private activity in one location may be offset by a low ratio in another location. Data can appear skewed if the consultant in question only has a small number of discharges during a reporting period, while there are challenges relating to the application of the process for consultants on short-term contracts as the reporting and monitoring is performed three months in arrears in line with HIPE coded data availability. Completeness of HIPE coding can have an impact on the overall compliance reported.
“These factors are taken into consideration in determining whether intervention and escalation is required,” according to the report.
“There is active management of non-compliance and hospitals are actively engaging with consultants with a view to continuing improvements in this area.”
No cases of consultant non-compliances were escalated to the National Director of Acute Operations in 2019.
Internal audit
In January 2020, the HSE’s Internal Audit Division reported to the National Director of Acute Operations on the effectiveness of the consultant contract compliance framework. The report included 10 findings and 13 related recommendations. At the time of the 2019 report’s completion, six recommendations were fully implemented, while seven were in in progress.
Those to be implemented include: Finalising the compliance guidance document; agreeing and implementing an approach to the measurement of outpatient and diagnostic activity (two recommendations); ensuring that the standard template for reporting is implemented across all Hospital Groups; ensuring work plans reflect Haddington Road Agreement commitment; annual declaration template to be drafted and reviewed by the Department of Health; and developing a detailed training module.
During 2019, HSE Internal Audit also carried out audits in seven acute hospitals. The audits were across four Hospital Groups and comprised three voluntary and four statutory hospitals. The main findings related to partial compliances in respect of work plan completion and processes for off-site compliance. The recommendations were all either implemented or in progress.
The issue of monitoring contract compliance was discussed at a meeting of the HSE’s audit and risk committee on 9 October 2020. The HSE National Director of Acute Operations Mr Liam Woods spoke about compliance framework and audit findings. The committee noted Mr Woods’s comments “on the delays that Covid has caused and that paradoxically compliance may have risen during this time; however, breaches could still be observed”.
Mr Woods answered questions regarding the consultant recruitment process and “the extent at which managing the existing contracts will inhibit consultant recruitment going forward”.
“He stated that the option to do private work may be an attractor and this is not currently an inhibitor,” according to the minutes.
The committee noted that 29 type C contracts, which allow for private work off site, had recently been approved.
Mr Woods clarified that the measurement of diagnostic and outpatient activity is complex and noted that work is being undertaken with HIPE to better understand “the division of work in this area between the public and private space”.
“He highlighted that outpatients is not a particularly vulnerable area to consultant contract compliance, while the biggest residual area of exposure is in diagnostics due to complications in measurement.”












Leave a Reply
You must be logged in to post a comment.