Consultant in Pain Management and Neuromodulation, Mater Private Hospital, Cork, Dr Dominic Hegarty highlights the benefits of bringing technology centre stage and personalising pain management
Pain, and the efforts to control chronic pain, is one of the most common reasons an individual attends their doctor. In fact, one-in-eight Europeans report pain on a daily basis. A MEP Special Interest Group, Pain Alliance Europe (PAE), has focused on this area. It now represents over 400,000 individuals in 19 different countries and it has have worked tirelessly to promote awareness over the last 10 years. This issue of chronic pain was initially championed by former Irish MEP Marian Harkin (TD). Over the years, PAE has published reports supporting the need for more resources and effective policies.
Its most recent document Brain, Mind and Pain (BMP) 2019, which was updated in February 2021, continues to identify that lack of awareness as the biggest challenge that the European community is facing when it comes to chronic pain. PAE also highlighted that improving education and awareness across all domains of society including employers, younger generations, policy-makers and healthcare professionals will be required to “reframe the economic and societal impact” of BMP disorders and are “essential steps towards ensuring greater social inclusion of people” with chronic pain.
Medtech
One thing the Covid-19 crisis has demonstrated is that the way we do everything can and needs to change. Technology has successfully provided the solution to many clinical issues over the last 12 months. But why did it take a pandemic to energise this change? Possibly the lack of knowledge, or perhaps the lack of confidence to rely on these solutions that proved to be the stumbling block pre-Covid. Ironically for more than a half-century, technology, in the form of neuromodulation therapies, has provided evidence-based alternatives to long-term drug therapy for the symptomatic relief of chronic pain. In Ireland, our economy has thrived on having the ability to provide innovation via the medtech sector.
The Irish Medtech Association reports that during the recent economic crisis (2016-2020) the medtech industry continued to expand, with exports reaching €12.6 billion. This steady growth, which accounted for more than 10 per cent of all Irish exports, bolstered the recovery in the domestic economy. It is likely we will need to rely on this area to perform as well in the future. Indeed, I have had the pleasure of being involved with several SME start-ups, and university based projects over the last 10 years and have seen the positive impact first-hand.
The innovation in the medtech sector has a key role to play in addressing the challenges that the global healthcare systems face. They have embraced the challenge of addressing clinical need and resolving real-time issues that matter. Industry has developed cost-effective solutions with long-term data in many conditions to support long-term solutions. The development of devices such as cardiac pace-markers, diabetic monitoring systems, urinary incontinence systems, and pain management are some simple examples.
Personalised pain management with technology
Pain is a personal emotional experience. While certain aspects of therapy are transferrable the key is to personalise therapy to ensure it has the greatest impact for each individual. The concept of personalised pain is a realistic target. In the field of pain management there are a growing number of nerve stimulation devices that would eliminate the need for the pharmaceutical options, which often comes with a host of other side-effects beyond addiction.
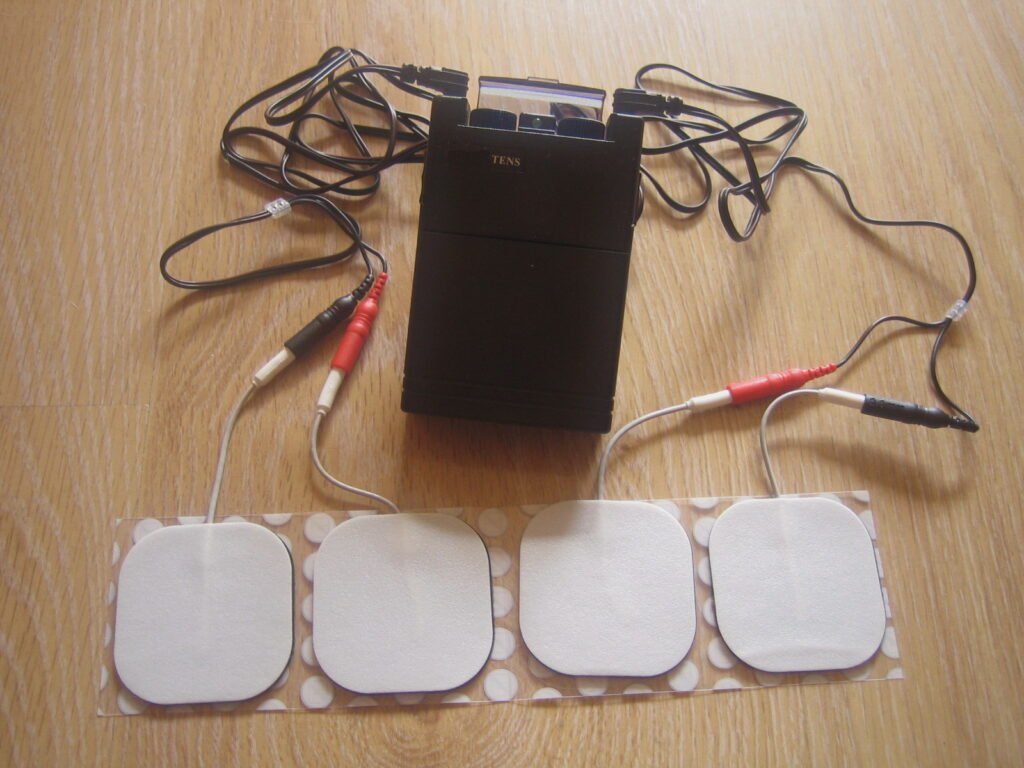
It works by providing a counter-current to block pain transmission. In principle Melzack’s and Wall’s “gate control theory” from 1965 still holds true. Therefore, you would be forgiven for thinking that the future looks rosy for chronic pain patients. But alas there is a sting in the tail. Despite the fact there are now more CE and FDA approved neuromodulation devices available, with years of clinical data and clinical experience to rely on, Irish pain clinicians still really have no choice when it comes to therapy.
The reason for this lack of choice lies squarely with the reimbursement practices and the lack of knowledge/interest in the area. This is the exact issue the PAE group identified in its report. The commercial payers, it seems, do not want to pay to have options in terms of neuromodulation stimulation. This is despite clinical and cost-effectiveness evidence supporting different types of devices in neuropathic pain indications. The same payers seem to suffer from the same mental blockage that held e-health care back for so long and yet the same payers are now promoting telehealth medicine as if it was their idea.
Neuromodulation has been shown to provide sustained improvement of 80 per cent, with minimal side-effects and huge patient satisfaction ratings and cost savings barely getting a look in
Stop the ‘black box’ process
Intriguingly whenever the insurers are asked to consider a device, even on a case-by-case basis, they invite the application and request all the information. They stall the process for months and then convene a ‘black box’ meeting to assess the application. In general, the conclusion is the same; that there is “not enough evidence-based data” to consider the therapy.
Yet there appears to be enough evidence globally to allow CE and FDA approval to use the equipment. There seems to be enough evidence globally to show the impact neuromodulation has on chronic pain. So what insight does the expertise in the insurance companies have to allow them assess the data so differently? It appears they never seem to engage a specialist in the area to even ask some background questions.
So without having to give any plausible reason or explanation, and with no appeal structure, the clinicians go back to their clinic to dole out more of the same therapy. As for the fee paying member, they will continue to pay the high insurance fees in order to access a system that keeps them on the long-finger while their counterpart in Europe or the US have access to treatment. The insurers get off scot-free while the solution to their members’ chronic pain sits neatly in a box on the shelf unopened.
So why are the insurers so afraid of technology? Are they afraid of a sudden uncontrollable explosion in implants that will result in a poor return for their shareholders? The time has come for meaningful and open discussion.
Is discussion too much to ask for?
Surely not. The evidence in favour of neuromodulation is substantial. We need greater access to neuromodulation therapy for individuals suffering from chronic pain, including some of the newest therapies targeting difficult-to-treat pain conditions. This expanded access would enable individuals obtain advanced, non-opioid stimulation therapy to treat nerve pain and other conditions due to complex regional pain syndrome or peripheral neuralgia etc.
I completely support the argument that any device must be is based on rigorous scientific research of stimulation therapy, and show that neuromodulation can provide meaningful improvements in health outcomes. The payer has a right to this to know what they are providing. The clinician, and most importantly the patient, have the right to treatment that works.
We must set realistic inclusion criteria, in order that the clinician can access the best device for the best candidate now. The insurers must remember they are all working in the area of healthcare. There is no on/off button to guarantee an outcome. The ‘one-size-fits-all’ mentality being imposed by the insurers is outdated. Interestingly, they seem happy enough to support ongoing medical management that may give a 30 per cent chance of helping individuals.
Neuromodulation has been shown to provide sustained improvement of 80 per cent, with minimal side-effects and huge patient satisfaction ratings and cost savings barely getting a look in. Pain clinicians want to be able to provide the most suitable and cost-effective treatments.
The concept of personalised pain therapy is not a far-fetched expensive aspiration. The shift in the arrangement should be controlled and rational. It should be towards offering the clinician choice in order to provide personalised pain management and delivering the care that is needed now, not in another decade. Insurance companies for their part need to realise that technology is here to stay.
With the well-publicised backlog in the healthcare system looming, surely having a solution that provides recognised cost-effective pain relief should be a target. It will take some of the high-end consumers out of the health cycle allowing time to deal with others. Bring technology centre stage and personalise pain management. This is a win-win situation.












Leave a Reply
You must be logged in to post a comment.