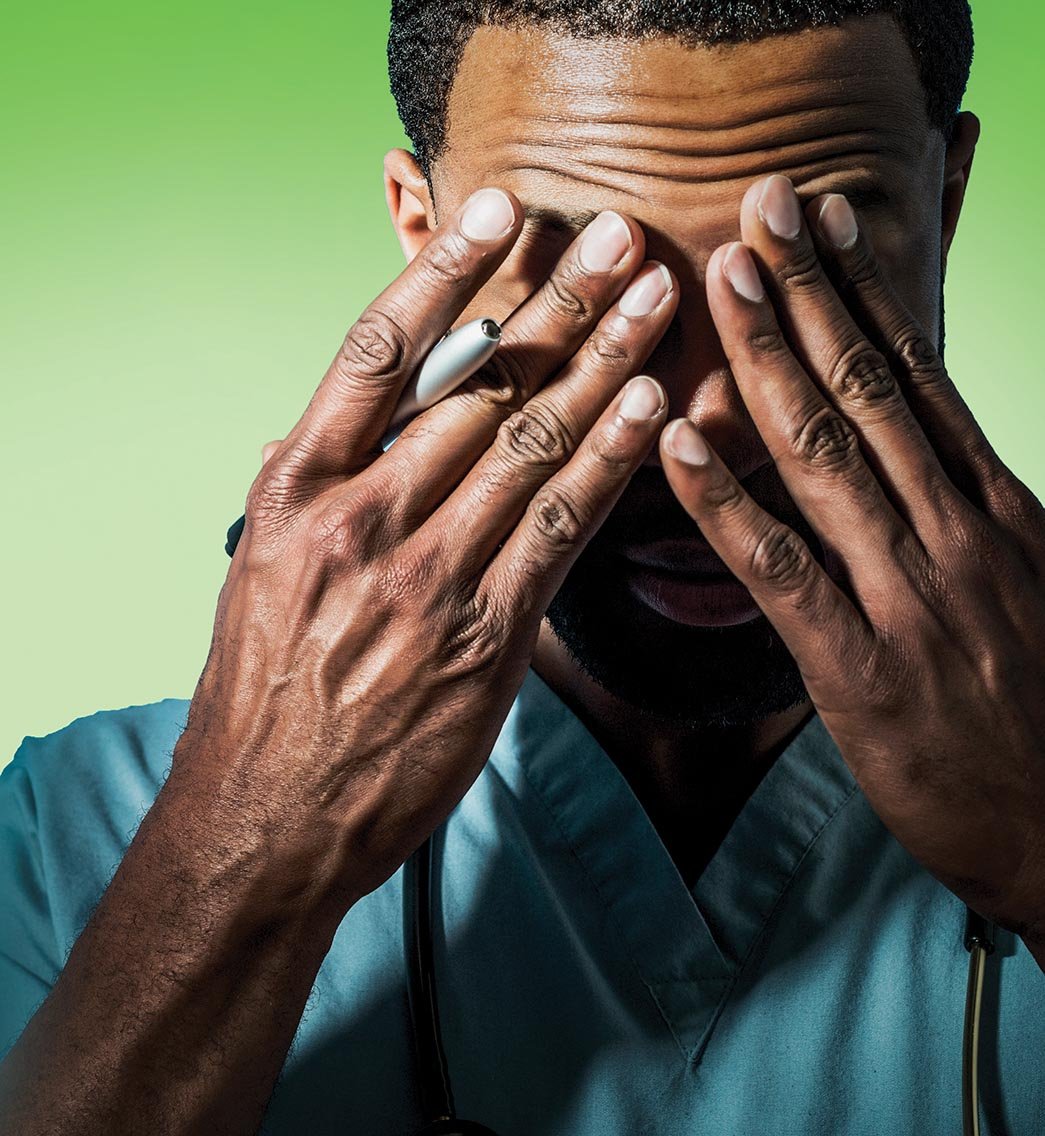
The excessive working hours faced by NCHDs has remained a major concern and continues to drive doctor emigration from Ireland.Catherine Reilly reports
On Twitter recently, Medical Council President Dr Rita Doyle stated that the European Working Time Directive (EWTD) “should be enforced” and “overworking” NCHDs was illegal.
“Interns and JHDs [junior hospital doctors] should be nurtured – they are the future of Irish medicine – overworking them is illegal,” tweeted Dr Doyle.
“The EWTD should be enforced and finally teams should be built to support each other. Doctors who are treated humanely will be good ‘human’ doctors.”

Her comments came in the wake of the Medical Council’s latest Your Training Counts report, which collected data in 2017. It found that over one-third of trainee respondents reported working 60 hours or more in a typical week.
Furthermore, trainees who worked longer hours were more likely to have been involved in an adverse event than those who worked fewer hours.
2013 agreement
Six years ago, NCHDs went on strike over dangerously long working hours, leading to an agreement with health service management that included a compliance verification group with IMO representation.
Under the agreement, shifts above 24 hours were to be eliminated by early 2014 and full EWTD compliance achieved during that year.
While some improvement is acknowledged, many NCHDs say progress has stymied and highly unsafe working hours remain a reality in the Irish health service.

In April, at the IMO NCHD committee’s national meeting, Chair Dr Paddy Hillery referred to “increasing stories” of junior doctors working shifts in excess of 36 hours.
Mr Anthony Owens, IMO Director of Industrial Relations (Consultants and NCHDs), told the Medical Independent (MI) its NCHD committee is “very concerned” about current working hours.
Mr Owens also confirmed to MI that the IMO has requested the Workplace Relations Commission (WRC) to undertake an evaluation of NCHDs’ working hours, due to concerns about the accuracy of data published by the HSE.
“I understand they have visited University Hospital Kerry and Beaumont. I don’t know the outcome of those visits because it is a process the WRC guards very closely, but I understand those visits have taken place,” stated Mr Owens.
A spokesperson for the Department of Business, Enterprise and Innovation told MI that the WRC “does not comment on individual cases or investigations”.
According to a HSE performance report in March 2014 (when these reports started including EWTD-related data), 93 per cent of NCHDs did not work more than 24 hours on-site on-call (not an EWTD target) compared to 42.8 per cent in March 2013.
Furthermore, 48 per cent of NCHDs were compliant with the 48-hour average working week in March 2014 as compared to 34 per cent in March 2013.
As of June 2019, HSE figures show compliance at 97 per cent for the 24-hour maximum shift and 83 per cent for the average 48-hour week.
The IMO conducted its own survey on NCHD working hours with findings published in its annual report for 2018.
Forty per cent reported working more than 24-hour shifts; over 80 per cent had worked more than 48 hours in a single week; and 35 per cent reported that the means by which working hours were recorded at their work site was not accurate.
The union said it seemed clear that hospitals were, in too many cases, “reporting roster compliance as opposed to actual working hours’ compliance”.
Nevertheless, there are significant deficits in compliance even within the HSE’s contested data.
According to July 2019 statistics held by the HSE, the percentage compliance with the 24-hour maximum shift (in the ‘all NCHDs’ category) was significantly below 100 per cent in the following cases: Roscommon University Hospital (55 per cent; as compared with 100 per cent in June); Children’s Health Ireland (CHI) at Tallaght University Hospital (67 per cent; and 64 per cent in June); CHI at Crumlin (75 per cent; the same in June); University Hospital Waterford (86 per cent; and 90 per cent in June);
At CHI in Tallaght, just 57 per cent of registrars had compliance with the maximum 24-hour shift (same in June) and only 33 per cent of specialist registrars and senior registrars (29 per cent in June).
Compliance with the 48-hour working week fared more poorly. In the category ‘all NCHDs’ for July, the figure was 54 per cent at Beaumont Hospital, Dublin (76 per cent in June); 63 per cent at St Vincent’s University Hospital, Dublin (same in June); 54 per cent at the Mater Misericordiae University Hospital, Dublin (56 per cent in June); 24 per cent at Mallow General Hospital (33 per cent in June); and 63 per cent at Bantry General Hospital (95 per cent in June).
Furthermore, just 17 per cent of interns at Beaumont were recorded as compliant with the 48-hour average week (compared with 70 per cent in June) and 36 per cent of interns at the Mater (compared with 76 per cent in June).
Of the 42 hospitals returning data to the HSE, St Columcille’s Hospital, Loughlinstown, Dublin; Cappagh National Orthopaedic Hospital, Dublin; University Hospital Kerry; and Roscommon University Hospital recorded their NCHD working hours as fully compliant with the 48-hour average working week in July.
Emigration
Your Training Counts found that of trainees considering practising medicine abroad, almost two-thirds were doing so because they felt their working hours in Ireland were too long, and this was the main predictor of wishing to emigrate.
The Twitter bio profile of Irish SHO Dr Ellen Newman warned that she would “emigrate for acceptable working conditions/pay/respect”. Earlier this year, she left Ireland to work in New Zealand.
According to Dr Newman, “every single week I worked back home was over 48 hours, with the exception of weeks I was on nights, or the three months I spent on rehab in Cappagh.”
While she personally did not work any 24-hour shifts, her understanding was that Tallaght had 24-hour shifts for interns and medical SHOs, the Mater had 36-hour shifts for surgical SHOs and Beaumont had 24-hour shifts for neuro SHOs and registrars, as examples.
The situation in New Zealand is very different.
“In New Zealand we’re scheduled Monday to Friday 8am-4pm, with call/nights/weekends additionally. We’re paid everyday as if we work 8-6pm, however it’s rare to ever do so. Call depends on your roster, and while some people may work a long weekday (8am -10pm) weekly, they might have no weekend shifts for that entire three-month period.
“However, we do not get paid extra the weeks we work on-call shifts etc that are rostered – because of the additional two hours we’re paid this averages out. A premium is offered to pick up extra shifts, cover weekends, etc. They were also very quick to offer locum rates for extra staff during the height of flu season too.”
One of the biggest differences noted by Dr Newman in New Zealand’s healthcare system is there is a member of HR solely assigned to resident medical officers (postgraduate year one-to-four).
“There’s a huge culture of feeling cared for and significant and not another cog. This means that we’re all happier to pick up extra shifts – because we don’t feel used and because we know we’ll definitely get the locum rate offered without having to fight for it.”
Dr Toby Gilbert, an Irish consultant in general medicine based in Adelaide, Australia, has a “steady stream of Irish NCHDs working for me and it would seem that implementation of EWTD has been patchy [in Ireland]”, he stated.
“I’m aware one would think all is rosy if one were to work exclusively off the official figures. There was, in my opinion, a flaw in the arrangement after the industrial action …The mechanism for the HSE to know about breaches was for NCHDs to fill in a form and the hospital would be fined.
“NCHDs have enough paperwork to complete daily and so form completion of course dropped off after a very short interval. Hospitals are incentivised not to report breaches, as they would be fined.
“In Australia, if the union wants a particular behaviour eliminated, then the contract states that the money ends up in the pocket of the doctor. So I can’t roster my NCHDs to work more than eight days in a row or every hour from day nine costs a large premium. Likewise if they are rostered for more than 69 hours in any seven day period. There’s a bonus if they work more than six hours and don’t get a meal break.”
Dr Gilbert said the maximum shift length is 13 hours including breaks and “they are aghast at 24+ shifts”.
“The IMO have always shied away from breaches of EWTD lining the pockets of the doctors doing the work. This is understandable: ‘Fat cat doctors’ trying to profit further could play poorly with the general public.
“But the discrepancy between the official figures and reality presents an opportunity. The IMO could argue in the LRC for premium payments for NCHDs that, were the HSE’s own figures true, wouldn’t cost the system too badly, but would help tidy up the last few hospitals in breach. The HSE couldn’t argue against that, and the hospitals would be put under direct financial pressure to improve NCHDs’ lot.”
Site visits
As well as requesting WRC involvement in evaluating doctors’ working hours, the IMO has recently contacted the HSE requesting a return to sites visited earlier this year, namely Waterford University Hospital, Cork University Hospital, and University Hospital Kerry.
This would be in order to assess “what improvements, if any, had taken place in those sites”, Mr Owens told MI.
“The concerns we had we still have, because we are concerned that we are seeing statistics that would suggest that we are a long way down the road to EWTD compliance, but we are not sure that that is the case. The anecdotal evidence we have is that we are still some way off.”
The IMO’s suspicion is that “the reporting mechanism is not capturing all hours that are worked”.
“We suspect it is because there may be additional forms that are required to be filled out, in order to capture all of the hours people are working. There is no central system that seems to be doing it.”
Mr Owens emphasised that it is “something we are going to dig deeper into”.
Asked in what manner this would occur, he responded: “Well we want to get accurate figures and we want to get back to where we ought to be, in terms of the agreement that was reached back in 2013, of people doing 48 hours tops and no more than 24 hours at a time.
“I think we will be looking to talk to the employer’s side about this on a national level just to try and get a read for these figures and see if there is anything we need to do to get them down,” added Mr Owens.
He also said the verification group “is not as active as it ought to be, in my opinion”.
On the Australian model, whereby the junior doctors’ contract instigates premium payments when working hours are breached, Mr Owens said it “is an interesting idea. I think when we do sit down with the employer and get into discussion on this, it is something we may find ourselves talking about.
“We’d probably need more information ourselves before we did that, but the concern we would have is that the incentives to get people, and to get NCHDs EWTD compliant, or certainly agreement-compliant, just don’t seem to be hitting home at the moment.”
Rostering will need to come under greater focus, according to Mr Owens.
“We probably need to have a consideration of handover times and so on. I always thought that was an issue, [in an environment where] people cannot just finish and leave, so maybe we need to look at how we are actually handling handover in practice.”
It may be the case that handover is responsible for a significant amount of breaches of the 24-hour shift.
“It certainly plays a part in it. But again, there is a service delivery element … you have 24/7 hospitals, people are going to be presenting needing care across the 24/7 period so there is a certain element of this being demand-led.”
On a related note, the transfer of tasks agreement, approved in 2016, was meant to help free-up NCHDs’ time to complete other duties and assist in reducing working hours.
However, Mr Owens said “progress is slower than we’d like it to be on that front…it is going to take some time. It should be happening quicker than it is, I am afraid.”
A Department of Health spokesperson told MI it has “ongoing contact” with the HSE in relation to progressing EWTD compliance for NCHDs.
“It is aware from the monthly data collected by the HSE that there are still some doctors who are working excessive hours, though significant progress has been achieved over the past five years in relation to eliminating shifts exceeding 24 hours and reducing the average working week to 48 hours or less in accordance with the Directive.
“This reflects the ongoing work of the national implementation and verification group, that includes HSE and IMO membership. Arrangements to ensure the accurate recording of protected training time is also being advanced by National Doctors Training and Planning (NDTP), HSE, in the context of implementing the MacCraith Group’s recommendations on supporting NCHD training,” they added.
EWTD compliance is “an important patient safety issue as well as a safety issue for individual professionals”, according to the RCSI.
“The RCSI would of course be concerned about trainees working excessive hours and we would continually advocate that the HSE responds to ensuring that there are appropriate resourcing of our hospitals, especially where there is a need for 24/7 surgical cover and that compliant levels of on-call rotas are adhered to,” said its spokesperson. “It would be very important that the HSE and hospitals accurately record EWTD compliance and where there are non-compliances that they would take steps to address these matters.”
The RCSI has not received reports from trainees of incidents of excessive working hours, according to the spokesperson.
“However, we are aware that incidents of excessive working hours occur and the RCSI has a process through which trainees and trainers can raise these concerns. While responsibility for compliance with the EWTD rests with the employer of our trainees, the RCSI can provide support to trainees and trainers in such circumstances and we can raise the matter with the HSE NDTP unit and HSE HR.”
According to the ICGP, its criteria for accreditation of GP training schemes include the trainees’ roster being EWTD compliant where a post has an on-call commitment.
“Individual training schemes satisfy the criteria by inspection of the hospital posts on a regular basis, usually every one-to-two years,” said the ICGP’s spokesperson. “It is the understanding of the ICGP that individual training schemes raise the issue of excessive working hours, when necessary, with the implicated hospital departments. Failure to address the issue can result in a post being demoted as being suitable for GP training.
“That hospital posts are being inspected and addressed appropriately is, in turn, a usual part of the accreditation process of the scheme by the ICGP. We have a multitude of reports on record confirming that the hospital post-inspection process is being conducted appropriately.
“The frequency of hospital post-inspection and the consistency of this happening across the country is protective for GP trainees against excessive hours of duty.”
The RCPI was also contacted for comment, but had not responded by press time.











Leave a Reply
You must be logged in to post a comment.