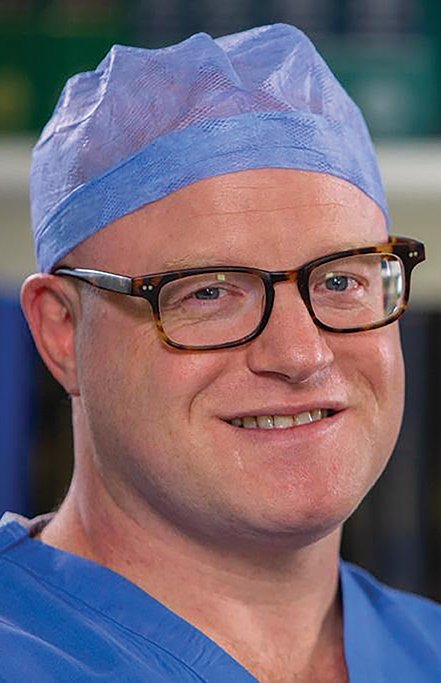
Catherine Reilly speaks to Consultant Transplant Surgeon Mr Tim Brown about organ transplant services in the North and innovations in the area
Some 40 out of 57 cadaveric kidney transplants in Northern Ireland in 2018 involved donation after cardiac death (DCD), with a leading Belfast transplant surgeon describing the DCD programme as “the biggest step forward” in the area.
Mr Tim Brown, Consultant Transplant Surgeon at Belfast City Hospital, told the Medical Independent that over 100 kidney transplants from DCD donors have taken place in the North to date.
While the transplant unit had been “stretched” in undertaking DCD transplants, Mr Brown said the national organ retrieval service was “very well resourced”.
There had been “a massive increase in the number of donors” in the UK over the past five years due to use of extended donor criteria and DCD, according to Mr Brown. “These are people that traditionally would never have been considered organ donors — people who’d used intravenous drugs, older donors, obese donors, people with multiple comorbidities and DCD.”
In January, Prof Jim Egan, Director of the HSE’s Organ Donation and Transplant Ireland (ODTI), told MI that use of extended donor criteria and DCD were being advanced, but the key challenges were resourcing and infrastructure. Due to the fall in road deaths and improved stroke care, for example, the donation model needs to evolve from the traditional donor pool. However, last year to 31 October, there were just four DCD donations in the Republic.
In the North, the turn-down rate on extended criteria donor kidneys has decreased to around 35 per cent.
“By doing that, what we have done is increased the risk profile of the transplant programme, but at the same time we have increased our cadaveric transplant numbers hugely,” according to Mr Brown. The downstream effect is the waiting time for a kidney transplant has gone from approximately 900 days to 400 days. The journey into extended donor criteria has also involved the use of 3D printing software to assist in preparing for a complex case, whereby a living donor had a tumour on his kidney.
Meanwhile, Mr Brown described a well-developed audit system in respect of monitoring donation opportunities in intensive care units (ICUs) and adequate specialist staffing in the area of organ donation. These are two areas highlighted by the Irish Kidney Association (IKA) as requiring much better development in the Republic.
Each of the nine adult ICUs in the North has specialist staff in organ donation, outlined Mr Brown. “In every intensive care there is a clinical lead for organ donation, that is usually a consultant anaesthetist, and there is at least one specialist nurse for organ donation… As well, there is a specialist nurse attached to the paediatric intensive care unit and there is a specialist nurse attached to the emergency department in the Royal Victoria Hospital — we could always do with more resources in terms of organ donation nurses, but there has been a lot of resource applied to this area over the last five years.”
In terms of age criteria, the oldest living kidney donor has been 82 and the oldest cadaveric kidney donor 79, with the organs “working extremely well”, added Mr Brown.
Last year, some 60 of the 117 kidney transplants undertaken in the North involved living donations (compared with 40 out of 167 kidney transplants in the Republic).
According to Mr Brown, the North has the highest number of living donors per million of population (42 per million) anywhere in the world.
“That has been achieved by the vision and drive of Dr Aisling Courtney, who is a consultant transplant nephrologist,” he said.
The protocol in the North includes a one-day assessment programme pioneered by Dr Courtney, “where she has eradicated donor fatigue.”
“When before, it used to take 12 months to assess and process a potential donor, now we can do that in one day.”
Mr Brown also alluded to huge potential in North/South collaboration in organ donation and transplantation. He said there have been “extensive conversations” to find out ways in which collaboration could be harnessed to benefit patients.
There is also work ongoing around finalising a memorandum of understanding to facilitate patients from the Republic having access to paired kidney exchange in Belfast.
“I can’t emphasise enough how open we are to cross-border work,” added Mr Brown, who said this must be pursued, irrespective of Brexit.
“There is an awful lot we can do by collaboration, border there or not, Brexit there or not.”
Mr Brown also stated his opposition to ‘opt-out’ legislation. This system does not pertain in the North, but has been mooted. The Irish Government plans to introduce ‘opt-out’ legislation in the Republic.
Rather than legislation, he emphasised the need to inform and educate populations around organ donation.
Organ Donor Awareness Week is currently taking place (30 March-6 April). It encourages the public to support organ donation by letting family know their wishes. For further information, visit the website of the Irish Kidney Association, www.ika.ie.











Leave a Reply
You must be logged in to post a comment.