The 2006 National Disability Survey Ireland (CSO, 2008) stated that pain was one of the most common disability types reported. Almost 50 per cent of individuals reporting pain as the main cause of their disability and of those, with 34 per cent indicating arthritis as being the most common cause of injury or illness. Almost 20 per cent stated the pain disability was caused by an accident or injury.
For the purpose of this article, I will discuss the types of acute pain often seen in community and GP settings. The management of acute pain from severe trauma (eg, RTAs) that requires management with likes of opioids and sedation in hospital settings is outside the scope of this article.
Causes of pain
The cause of pain is sometimes difficult to determine and there are often many aspects to consider. Chronic pain can be more difficult to determine the cause; acute pain more often has a more clearly identifiable cause, eg, muscle injury. It is the indeterminate nature that can present the biggest obstacle to health professionals to establishing proper diagnosis of the condition.
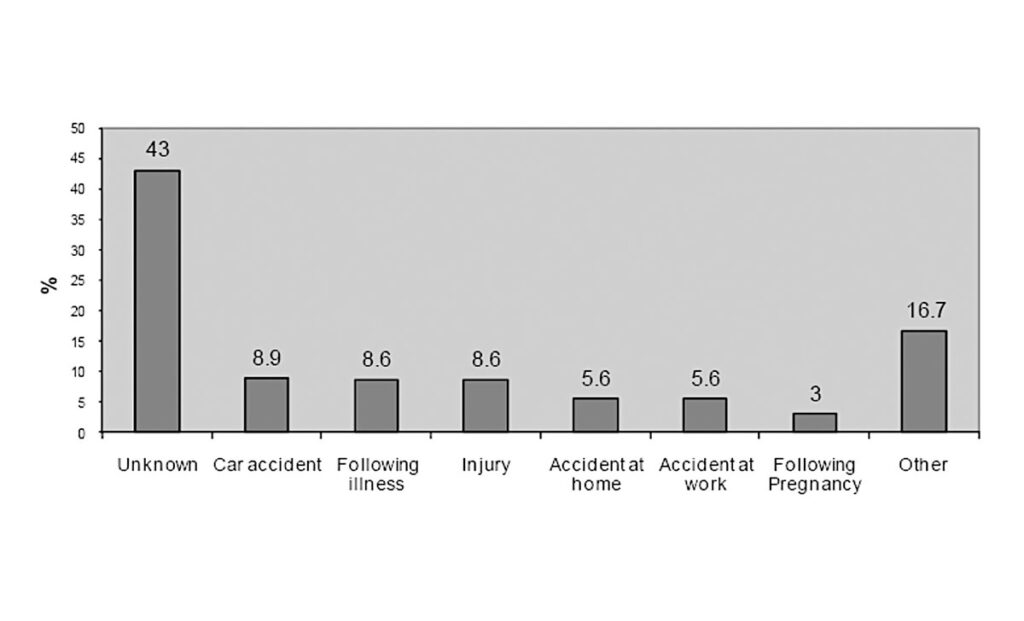
Figure 1 on reported causes of pain from the PRIME study, National University of Ireland Galway (NUIG) 2011, illustrates the problem further.
Acute pain
Acute pain starts quickly and lasts a short period of time. The definition of acute pain is pain that improves within one-to-three months of onset. Pain that lasts longer than six months is considered chronic pain and will require more specialist treatment from a pain expert. The period between three and six months is classified as the time of transition from acute pain to chronic pain. Patients require more specialist evaluation and treatment at this stage rather than just taking painkillers to avoid transitioning into chronic pain.
Common examples of acute pain:
- Headaches;
- Sprains and strains;
- Dental work;
- Surgery;
- Broken bones;
- Burns or cuts;
- Childbirth.
Acute pain can be difficult to diagnose and treat, especially when caused by injuries that are not visually evident like a fractured rib, a herniated disc, or a pinched nerve. Pain can develop to be more than a physical sensation. For example, it can develop to become an emotional problem, such as fear, or anxiety related to a traumatic event that triggered the pain. For example, a person may avoid driving after suffering severe injuries in a car accident.
Reasons for acute pain
The majority of acute pain episodes arise from causes that can be categorised as musculoskeletal conditions.
Pain is a sensation experienced through the nervous system (nerves, spinal cord, and brain). Reflexes are the nervous system’s immediate response to acute pain. This is demonstrated by when a hot plate is touched, it takes milliseconds for the nervous system and muscles to coordinate and make the hand move away immediately; ie, a reflex reaction.
In addition to reflexes, the nervous system has more sophisticated mechanisms for processing pain. The brain releases neurotransmitters that influence pain levels and have an influence on mood, which is one of the reasons why depression can occur in response to pain. Pain and depression can create a vicious cycle in which pain worsens the symptoms of depression and then the resulting depression worsens feelings of pain.
Symptoms of acute pain
Acute pain can be felt in a specific body area, such as the neck or back, or the patient may have widespread pain with conditions, such as a viral illness.
Acute pain may be described as:
- Sharp;
- Dull;
- Stabbing;
- Throbbing (sign of inflammation);
- Shooting or shock-like (sign of nerve involvement).
Diagnosis for acute pain
The reason for the pain may not be visually obvious. Diagnostic tests are helpful and include:
- Blood tests;
- Imaging studies (x-ray, CT, MRI, nuclear scans);
- Local anaesthetic injections;
- Dye-injection studies, such as a diskogram to identify painful disks in the spine or myelogram to identify areas of spinal nerve compression;
- Electromyography and nerve conduction studies to identify nerve abnormalities.
Chronic pain versus acute pain
Chronic pain can be defined as pain which lasts longer than what is considered a ‘normal’ healing time, perhaps as part of recovery from illness or injury – generally more than three months.
Chronic pain may be attributable to an event, such as an accident, developing from acute pain. Opinion differs as to whether previous acute pain is always the root cause of chronic pain or simply appears, sometimes without an initial cause. In some cases, especially in relation to sports injury in contact sports, the underlying chronic pain may appear sometime after an event. Pain may also be related to another condition. Surveys show that in Ireland, 35 per cent of reported chronic pain was arthritis related. It may site-specific, ie, back, knee, and wrist, however, 80 per cent of sufferers in Ireland report that their pain relates to more than one site.
Types of chronic pain
Pain can be classified either by type of pain, or by body region. Pain types include:
- Nociceptive pain: Aching, boring, worse on movement, anatomically defined, fluctuates in severity.
- Neuropathic pain: Burning sensation, sharp stabbing type, tingling, transient limb pain (shooting), associated with allodynia (experience of pain from a non-painful stimulation of the skin, such as light touch), hypersensitivity, or other sensory changes.
- Mixed nociceptive and neuropathic pain: Combination of symptoms.
- Visceral pain: Dull, non-specific, difficult to pinpoint.
- Autonomic symptoms: Physiological changes (colour, temperature), sweating.
Treatment
Aims of treatment are to:
- Reduce intensity of the pain;
- Enhance physical functioning;
- Improve mood;
- Promote the return to work or school and/or role within family and society;
- Improve quality-of-life;
- Support pain-management planning decisions;
MUSCULOSKELETAL
- Osteoarthritis
- Rheumatoid arthritis
- Osteomyelitis
- Osteoporosis
- Ankylosing spondylitis
- Myofascial diseases
- Polymyalgia rheumatica
- Polymyositis
- Fractures
- Chronic or repetitive overuse
- Carpel tunnel syndrome
- Muscular strains
- Faulty posture
- Mechanical low-back pain
HEADACHE AND/ OR MIGRAINE
- Cluster headaches
- Migraine
- Trigeminal neuralgia
- Giant cell (temporal) arteritis
- Glaucoma
- Smoking
- Alcohol
- Temporo-mandibular joint dysfunction
- Drug or substance overuse or misuse
NEUROLOGICAL
- Diabetic sensorimotor polyneuropathy (up to 25 per cent of diabetics)
- Spinal stenosis
- Brachial plexus traction injury
- Thoracic outlet syndrome
- Post-herpetic neuralgia
- Multiple sclerosis
- Alcoholism
- Thyroid disease
- Pernicious anaemia
- Infections (ie, HIV), polyneuropathies
- Polyradiculopathies
PSYCHOLOGICAL CAUSES
- Depression
- Anxiety
- Personality disorders
- Sleep disturbances
- Reduce need for healthcare services.
First-line treatment options include:
- Resting the affected area;
- Applying ice or heat;
- Paracetamol or non-steroidal anti-inflammatory drugs (NSAIDs) such as aspirin, ibuprofen, or naproxen;
- Exercise;
- Physiotherapy;
- Stress reduction;
- Bioelectric therapy (ie, local electrical stimulation like a TENs machine for moderate pain);
- Opioid medication, such as codeine or morphine;
- Muscle relaxant medications.
- Second-line treatment options include:
- Antidepressants: Some tricyclics such as amitriptyline have a role in nerve pain and some antidepressants may be needed for mood and insomnia issues exacerbated by pain;
- Anticonvulsants: More often used f or nerve pain;
- Nerve blocks: Local anaesthetics to block nerve activity;
- Trigger point injections: To treat muscle spasms;
- Steroid injections: To reduce tissue inflammation.
Overview of pain medications
A successful outcome from general practice visits should be a pain management plan. It is highly likely that as part of this, some form of pain-relieving medication will be prescribed. Ideally, advise on promotion of self-help, self-management, and other treatments to help improve their condition and add value to the benefit offered by medication.
Given the wide and varied nature of acute and chronic pain, there is a myriad of medication options. The effectiveness of medication depends on the nature and severity of the pain.
Regarding treatment of acute pain caused by headache (ie, migraine), in addition to standard paracetamol and NSAIDs, triptans are considered the most effective to combat acute attacks if ordinary analgesics do not work.
These include:
- Almotriptan;
- Frovatriptan;
- Sumatriptan;
- Zolmitriptan;
- Eletriptan;
- Naratriptan
All are prescription-only medicines (POM), apart from sumatriptan, which has an over-the-counter (OTC) version available in Ireland.
Efficacy of OTC painkillers
Cochrane reviews (39 in total) of randomised controlled trials on effectiveness of OTC analgesics in acute pain found reliable evidence to indicate that simple, inexpensive, and common analgesics give good pain relief to many patients with acute pain, such as headache, toothache, sprains, and strains. Data demonstrated the most efficacious OTC drugs used were ibuprofen/paracetamol combinations in respective 400mg/1,000mg and 200mg/500mg doses.
These formulations gave effective relief in seven-out-of-10 patients. Fast-acting ibuprofen 200mg and 400mg was effective in at least five-out-of-10 patients. Paracetamol alone was effective in four-out-of-10 patients.
World Health Organisation (WHO) analgesic ladder
The WHO analgesic ladder (introduced in 1986) was developed to help clinicians decide cancer pain treatment. It was developed for chronic pain, but the principles apply to the management of acute pain. OTC painkillers can be used for mild pain according to this tool, starting with a non-opioid (eg, paracetamol or aspirin) for mild pain then trialling an opioid plus a non-opioid (eg, co-codamol) for mild-to-moderate pain. Despite its origin to manage cancer-related pain, the WHO analgesic ladder now acts as a useful guide for pain control in both acute and chronic pain from malignant and non-malignant causes. As pain is a subjective experience, the stepwise approach of the WHO analgesic ladder is not always appropriate for managing intense pain.
Guidance on musculoskeletal injures
The American Academy of Family Physicians (AAFP) and American College of Physicians (ACP) guidelines published in 2020 (after a review of 13 million patients) recommend topical NSAIDs as first-line therapy for patients experiencing pain from musculoskeletal injuries (excluding lower back pain). The guidelines recommend that clinicians not prescribe opioids except in cases of severe injury or if patients cannot tolerate first-line therapeutic options.
The recommendations state that topical NSAIDs were the only intervention that improved all outcomes in patients with acute pain from non-lower back musculoskeletal pain. They found that topical NSAIDs also were among the most effective options for treatment satisfaction, pain reduction, physical function, and symptom relief, and were not associated with a statistically significant increased risk of adverse effects.
Oral NSAIDs were shown to be effective in reducing pain within two hours and one-to-seven days after treatment and were associated with greater likelihood of symptom relief. However, oral NSAIDs also were associated with an increased risk of gastrointestinal adverse events.
Self-help
Pain management programme
The Pain Management Programme (PMP) is a psychologically based rehabilitative treatment for people with persistent pain. It is delivered in a group setting by a multidisciplinary team of experienced healthcare professionals working closely with patients. The main aim is to teach a group of patients with similar problems about pain, how best to cope with it, and how to live a more active life. Referral to a PMP is usually through the GP to the local pain clinic.
There are public PMPs in*:
- St Vincent’s University
- Hospital, Dublin.
- Tallaght University Hospital, Dublin.
- Mater Misericordiae University Hospital, Dublin.
- Mercy University Hospital, Cork. *This list not exhaustive
Private hospitals also have pain clinics. For example, the Beacon Hospital in Dublin operates an acute pain service and a chronic pain service.
Physical therapy
Physical therapy covers a number of different treatment types, which can be beneficial for chronic pain, especially pain due to musculoskeletal disorders.
- Hot or cold (ice) pack treatment;
- Ultrasound;
- Peripheral nerve stimulation/transdermal electronic nerve stimulation (TENS).
A chartered physiotherapist can help with manual therapy, which helps to increase tissue extensibility and range of movement, thereby decreasing pain. Manual therapy can also help with alignment and joint mechanics issues, which in itself can also help alleviate pain.
Therapeutic exercise – such as hydrotherapy, can restore joint movement and flexibility and strengthen and condition muscles to help movement, thereby reducing pain.
Patient education – Can support physical therapy in a self-help or home-based manner. Reading and learning about their condition can assist in management of their own pain.
Exercise – Staying active can be the key to improving chronic pain symptoms. Any activity that increases mobility can have not only a positive physical benefit, but also an affirming mental health benefit also.
Cognitive behavioural therapy (CBT)
CBT is a proven ‘talk therapy’, the primary aim of which is to teach the patient how to recognise and manage negative thinking or unhelpful beliefs that lead to increased distress. Generally delivered on a one-to-one basis, the participant is taught techniques and strategies to enable them to challenge their thoughts and change their attitude, leading to a change in future behaviour. Through regular attendance, confidence builds, leading to positive goal setting. These goals should relate to achieving resumption of activities previously restricted by pain.
Learning problem-solving strategies and stress reduction techniques will help achieve a successful outcome.
General practice
The patient’s needs will affect treatment choice so GPs and primary care teams should have available (and understand) a range of guidance and literature to best advise patients about the most effective treatment for them.
Regular review of the continued suitability of all medications used by those with both acute and chronic pain is vital. For many, beyond the pharmacy, the GP surgery is the first port of call when a pain-related problem arises. Using some of the ideas regarding questions, pain diary, etc, will really help in enabling people to make better-informed decisions about their own next step. Becoming familiar with local resources like physios, support groups, condition-specific charities, etc, and signposting these will only add value to a positive perception.
| PAIN TYPE | EVIDENCE-BASED RECOMMENDED ANALGESIC |
| Lower back pain | NSAIDs, (eg, ibuprofen 400mg three times per day) at the lowest possible dose for the shortest possible time. Do not offer paracetamol alone |
| Tension-type headache | Aspirin (300mg three times per day), paracetamol or NSAID, taking account of patient preference and comorbidities |
| Migraine (must be medically diagnosed before OTC medication can be recommended) | Combination of triptan (eg, sumatriptan no more than two 50mg tablets in 24 hours), NSAID or triptan, and paracetamol. If the patient prefers one drug only, consider monotherapy with oral triptan, or NSAID (eg, ibuprofen) or paracetamol alone, considering comorbidities. Opioids should not be used for the acute treatment of migraine |
| Sprains and strains | Paracetamol (500mg to 1g four times per day, with a maximum 4g in 24 hours) or topical NSAID (eg, ibuprofen or diclofenac gels) are recommended first-line. Consider oral NSAID (eg, ibuprofen 400mg three times per day) 48 hours after the initial injury if needed |
| Period pain | NSAID (eg, ibuprofen or naproxen) unless contraindicated. Paracetamol can be used if a NSAID is contraindicated or provides insufficient pain relief |











Leave a Reply
You must be logged in to post a comment.