Case Study
A 45-year-old man who has sex with men (MSM) presented to a sexual health service requesting a sexual health screening; he had never been screened before. He did not remember if he had been vaccinated against hepatitis A or B in the past. As is currently routine practice, he gave a urine sample and had a rectal and pharyngeal swab testing for gonorrhoea and chlamydia. He had blood drawn for HIV, syphilis, hepatitis A, hepatitis B and hepatitis C.
Two weeks later, he presented for his results. There was no evidence of gonorrhoea or chlamydia, hepatitis B (HBV), hepatitis C, syphilis or HIV. His hepatitis A tested positive. This would not be unusual in this cohort and most likely represented past asymptomatic infection, maybe in childhood. As he was an MSM, he fell into the high-risk category for HBV, and vaccination was proactively encouraged. As per protocol from the most recent immunisation guidelines for Ireland, available on the RCPI website, he was started with a HBV vaccine. Follow-up vaccines were arranged one month later and six months after the first. Two months after the last vaccine, he returned to have a HBV antibody titre blood. This showed that he did not respond to the initial schedule, as his titre level was less than 10mIU/ml of blood.
This man was a HBV vaccination ‘non-responder’. As such, he had no protection against HBV. He was offered a further course of vaccines, this time a double dose, one in each arm at the elected date, one month later and at six months. This time, he had a HBV titre blood drawn and his anti-HBV antibody was greater than 100mIU/ml blood. He had an adequate response to vaccination and needs no further intervention.
According to the World Health Organisation (WHO), in July 2017 there were more than 257 million people chronically infected worldwide with the hepatitis B virus (HBV).
HBV is a potentially life-threatening cause of hepatitis and is a major global health problem causing chronic infection, which can result in cirrhosis and liver cancer. Areas of high prevalence (>8 per cent of the population) include sub-Saharan Africa, South-East Asia, the Pacific islands and the Caribbean. HBV is moderately common (2-7 per cent) in South Central and South West Asia, Russia and Central and South America. In Australia, New Zealand, North America and Western Europe, the prevalence of chronic HBV is <2 per cent. In Ireland, the seroprevalence of HBV infection is <1 per cent.
HBV is a notifiable disease in Ireland and as such, all medical practitioners, including clinical directors of diagnostic laboratories, are required to notify the Medical Officer of Health (MOH)/Director of Public Health (DPH) of new cases of HBV. These notifications are analysed by the Health Protection Surveillance Centre (HPSC) and annual reports are published on the website www.hpsc.ie. In 2016, 488 cases of HBV were notified to the HPSC. That was down on the 2015 figure (548 cases), but according to the HPSC epidemiologists, this represents a levelling-out of annual notifications, not a true decreasing trend. A total of 7 per cent of the notified cases in 2016 were acute hepatitis, where 93 per cent were chronic HBV infection. The high notification of chronic cases reflects people migrating from countries where HBV is endemic.
Co-infection with other blood-borne viruses, such as hepatitis C and HIV, can lead to more severe liver disease and an increased risk of liver cancer in people with HBV infection. Four HBV cases notified in 2016 were co-infected with hepatitis C and 13 additional cases were co-infected with HIV. Other sexually-transmitted infections were also reported for some of the cases of HBV notified in 2016. Five had recently been diagnosed with chlamydia, three with syphilis (two HIV positive), one with gonorrhoea and one with genital herpes simplex (HIV positive).
Epidemiology
HBV is a double-stranded DNA virus belonging to the <em>hepadnaviridae</em> viral family. The whole virus consists of an inner core and an outer surface coat. The inner core contains genetic material (DNA), DNA polymerase, an enzyme essential for reproduction, the core antigen and the e antigen. The whole genome is 32kb long. This genome is very small and HBV uses overlapping reading frames that encode four different proteins that make up the intact virus. During viral replication, viral proteins are combined to form intact viruses. Some of the viral proteins are synthesised in excess of the amount used to form infectious virions. These are empty viral particles that do not contain the genetic material of HBV.
These empty particles form the basis of the laboratory assay HBV surface antigen (HBsAg) and HBV infection is diagnosed by testing for these empty viral particles.
Transmission
Transmission of HBV occurs mainly by sexual contact, particularly anal and vaginal intercourse. Having another sexually-transmitted disease resulting in a breach of the genital mucosa at the time facilitates infection with HBV. Perinatal transmission occurs in 70-to-90 per cent of cases where the mother is infectious. HBV can live outside the body for a week or more, so percutaneous exposure, such as sharing needles in the setting of intravenous drug use is a key infection risk. Sharing toothbrushes and razors, piercing and tattooing can also result in HBV infection. Occupational and non-occupational needle-stick injury with blood from a source that has infectious HBV will result in infection without intervention in 30 per cent of cases. Transfusion-related HBV infection is rare in the developed world.
Once infected with HBV, there are three possible outcomes: Recovery (90-to-95 per cent); fulminant liver disease with a rapid decline in liver function and death (1 per cent); and chronic infection.
Infection
Serological markers of HBV are available to diagnose HBV. Testing determines whether the person is infected with HBV; if so infected, whether the infection is acute or chronic; and if not infected, whether protective antibodies exist.
There are three antigenic determinants associated with HBV infection, hepatitis B surface antigen (HBsAg), hepatitis B core antigen (HBcAg) and hepatitis B e antigen (HBeAg) and three corresponding antibodies — anti-HBs, anti-HBc and anti-HBe.
Chronic infection is defined as detectable HBsAg in the blood for more than six months.
HBsAg appears in the blood from about six weeks after an acute infection, usually before jaundice is clinically evident. Its presence indicates current infection or a chronic infection, as well as a carrier state. The presence of HBsAg in the serum indicates HBV infection and all HBsAg-positive persons should be considered infectious. A carrier is defined as someone who is HBsAg-positive on at least two occasions, at least six months apart. In persons who recover from HBV infection, HBsAg disappears from the blood and anti-HBs develop. Its presence in the serum indicates immunity from HBV infection following natural infection or vaccination.
HBcAg does not circulate in blood and does not appear on the laboratory results.
Its corresponding antibody, HBcAb, appears at the onset of liver test abnormalities and persists for life. Acute or recently-acquired infection can be distinguished by the presence of immunoglobulin M (IgM) class of anti-HBc and can persist for up to six months if the disease resolves.
The HBeAg may be detected in the serum of patients with acute or chronic infection. It is a measure of viral replication and infectivity. Its persistence correlates with the development of chronic liver disease and its loss correlates with low levels of viral replication. Certain HBeAg-negative individuals have high measurable HBV DNA levels (viral genetic material) suggesting high viral turnover. This is due to a mutation in the precore region of the HBV genome and results in failure to produce HBeAg, even in the presence of active viral replication. This is known as the ‘precore mutant’ HBV. Anti-HBe appears in the blood after the disappearance of HBeAg and correlates with low infectivity.
Screening tests
When screening for HBV infection, one needs to know three things: Has the person been vaccinated in the past, or has the person been infected with HBV, and if so, has the person cleared the virus or not? Anti-HBc (anti-hepatitis B core antibody) and HBsAg should be requested, unless the person has been vaccinated already. If the anti-HBc is positive, it means that the patient has had past exposure to HBV and may or may not have active infection at the time of phlebotomy. If the HBsAg is positive, it indicates that the patient is actively infectious and the infection may be acute or chronic. Patients have an approximately 90 per cent chance of clearing the virus and in this case, the HBsAg will be negative. The anti-HBc will, however, remain positive, indicating past infection and that vaccination is not warranted. If the anti-HBc IgM is positive, it will distinguish between acute and chronic HBV infection. A positive anti-HBc IgM indicates acute infection.
The laboratory, in the event of a positive HBsAg result, will perform further serological tests, ie, the HBeAg and the anti-HBe. These tests indicate the degree of infectivity or active viral replication. If the HBeAg is positive and the anti-HBe is negative, it suggests that there is active viral replication and that the patient is highly infectious and the likelihood of viral clearance is small. Similarly, if the HBeAg is negative and the anti-HBe is positive, it indicates that the active infection will most likely have a chronic low-level viraemia.
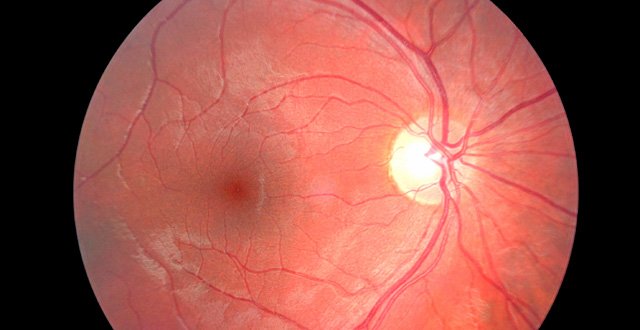
The gold standard for staging of liver disease is a liver biopsy. Patients with acute hepatitis are rarely biopsied. Microscopic appearance of the liver of a patient with active cirrhosis shows portal tract inflammation and interface hepatitis, normal bile ducts, lobular inflammation with ground glass hepatocytes present and negative special stains for iron, alpha-1 antitrypsin antibodies and copper-associated proteins. Transient elastography is also used to assess the degree of liver elasticity — which decreases as HBV infection progresses — fibrosis, cirrhosis and hepatocellular carcinoma.
The most common laboratory tests performed on patients in whom there is a clinical suspicion of viral infection aside from serology are liver enzymes. Serum ALT (alanine transferase) alone, or in combination with other liver enzymes, is not sufficient to detect chronic viral hepatitis in patients with risk factors for the disease. Furthermore, the correlation between the magnitude of enzyme elevations and the degree of liver injury is poor. Elevated liver enzymes may indicate the presence of the disease, but not the degree of liver damage. Other liver function tests available are the prothrombin time and serum albumin, both of which are an indicator of the liver’s synthetic capacity and the serum bilirubin, a measure of the liver’s functional capacity. Unfortunately, these tests may only become abnormal only after severe liver damage has occurred. Patients with chronic HBV are screened regularly for hepatocellular carcinoma in the setting of chronic HBV and cirrhosis with ultrasonography and alpha-fetoprotein measurement.
The incubation period of HBV ranges from 45-to-180 days, on average 90 days. Most infections are sub-clinical or patients may present with malaise, fatigue, anorexia, abdominal discomfort, nausea or vomiting. Patients may present with arthralgia or rash and 30-to-50 per cent of adults will have jaundice.
Diagnosis and treatment
For many, a diagnosis of HBV is made on routine screening.
There is no specific treatment apart from supportive measures for patients with acute HBV.
Chronic HBV can be treated with oral antiviral agents. In 2015, the WHO recommended tenofovir or entecavir as first-line agents for the treatment of HBV. Antiviral agents reduce viral replication in the liver, can reduce or slow the progression of cirrhosis and reduce the incidence of liver cancer. In the majority, treatment does not cure HBV, but only suppresses the viral replication.
Vaccination
A vaccine against HBV has been available since 1982 and is 95 per cent effective. The vaccine contains recombinant HBsAg. It does not contain live organisms and is not infectious.
In Ireland, it has been recommended by the National Immunisation Committee of the RCPI that certain groups should receive HBV vaccine if non- immune. These include doctors, nurses, dentists, midwives, laboratory staff, cleaning staff, general assistants and anyone who is at particular risk through contact with blood or body fluids. Others who should be vaccinated include the sexual and household contacts of acute cases of HBV; families adopting children from countries with a high prevalence of HBV; babies born to mothers with chronic HBV; people with haemophilia and others requiring regular blood transfusions; patients with chronic renal failure with poor immunity and who may require dialysis; and patients with chronic hepatitis. It is also recommended that security and emergency personnel, intravenous drug users, MSM, tattoo artists, and immigrants from and travellers to an area with a high seroprevalence of HBV are vaccinated too.
The standard vaccine schedule is three vaccines — one at the elected date, one a month later and the third at six months. Accelerated schedules are used in certain circumstances. It is recommended that two months after the last vaccine, a post-vaccination anti-HBs titre be checked. The level is reported in mIU/ml blood. A level greater than 100 is an adequate response and in an immunocompetent cohort, should last for life. A level of 10-to-99, a poor responder, warrants a booster dose and no further action, while those with a level of less than 10 are non-responders. Factors that might suggest that a person will be a non-responder include male sex, age over 40 years, increased body mass index, immunodeficiency and smoking. A further course of a double-dose vaccine, one injection in each arm, is recommended at zero, one, and six months for non-responders. This revaccination schedule is highly effective in inducing seroconversion. Failing seroconversion, patients need to know that despite vaccination, they have no defence against HBV and would need immunoglobulin in the event of a future exposure.
To confirm, the vaccine does not contain infectious HBV but only HBsAg. It does not contain HBcAg, so one does not make antibodies to HBcAg with vaccination. HBcAb are only positive following natural infection.
References on request
Dr Shay Keating, Associate Specialist in Sexual Health and HIV, St James’s Hospital, Dublin, and Harold’s Cross Surgery, Dublin 6












Leave a Reply
You must be logged in to post a comment.