The constellation of prolonged Covid-19 symptoms is referred to as ‘long Covid’ or post-acute sequelae of SARS-CoV-2 infection (PASC)
With the Covid-19 pandemic evolving into an endemic strain, there is a growing urgency to look beyond Covid-19 mortality figures to morbidity related to the increasing number of patients with ongoing symptomatic sequelae from acute SARS-CoV-2 infection. Clinical experience following the MERS and SARS coronavirus outbreaks meant a high likelihood of significant chronic symptomatology following the current novel coronavirus infection.
Studies have already shown a higher probability of prolonged symptoms post-Covid when compared to MERS,SARS or influenza. In one study looking at 270,000 survivors, 42 per cent had at least one symptom six months after acute Covid-19 infection compared with 30 per cent of post-influenza patients. The constellation of prolonged symptoms is referred to as ‘long Covid’ or post-acute sequelae of SARS-CoV-2 infection (PASC).
To date, over 500,000 people in Ireland have been diagnosed with Covid-19 (HPSC data, Nov 2021). Long-term follow-up data is increasingly robust and confirms that long Covid/PASC phenomena are increasingly recognised. Several definitions have been proposed for long Covid, including the presence of any symptom one, two, five or six months after an acute, objectively confirmed or clinically-likely Covid-19 infection. For this review, we have focused on studies that include symptoms at six months.
Current evidence
The growing body of long Covid research suggests the current number of patients attending post-Covid follow-up is only the tip of the iceberg. The most extensive systematic review to date of 57 studies looking at 250,000 Covid survivors showed that one-in-two patients had evidence of PASC, especially pulmonary, mental health, and neurologic disorders. Fatigue was frequently the most common, most severe, and most prolonged symptom.2 PASC was frequently not related to the severity of the initial acute infection. A similar prevalence has been reported amongst patients managed in community and hospital settings.
The most common respiratory problems were dyspnoea, cough, and increased oxygen requirements. Chest imaging abnormalities were surprisingly common, with a median of 62.2 per cent. Despite this, the absence of thoracic imaging abnormalities does not rule out long Covid. Cardiac symptoms mainly were chest pain and palpitations. Reassuringly, long-term structural cardiac damage occurred rarely.
Critical aspects of executive cognitive function can remain impaired more than six months post-Covid in another study. Abnormalities studied included impairments in processing speed, category fluency, memory encoding, and recall, which could explain the ‘brain fog’ typically described by survivors. Autonomic dysfunction was highlighted in 14 of 675 patients with PASC from the UK. This is a rare feature not mentioned in the earlier JAMA review. Patients in this UK study were referred to a cardiovascular autonomic specialist clinic for definitive diagnosis and follow up.
Reassuringly, a longitudinally planned study from Holland showed most patients did report a gradual improvement in all organ systems affected. However, a significant number of persisting symptoms remained at six months.3 More data is awaited from ongoing prospective studies with longer follow-up periods, including the CO-FLOW Dutch trial, which is following a cohort of more than 500,000 patients for up to two years after acute infection.
PASC/long Covid symptoms
- Breathing difficulties/dyspnoea;
- Fatigue/malaise;
- Chest/throat pain;
- Headache;
- Abdominal symptoms;
- Myalgia;
- Cognitive symptoms;
- Anxiety/depression
Pathobiology and pathophysiology
It remains unclear why long Covid occurs. In the Erasmus study, it was noted that Covid survivors had a sustained humoral response after Covid-19 infection. AntiSARS-CoV-2 IgM antibodies were detectable in 36 per cent of patients at six months, and 78 per cent of this same cohort had already been noted to have IgM antibodies at six weeks. Hence there was a gradual reduction between six weeks and six months.
Initially, anti-SARS-CoV-2 IgM was used as a marker of acute infection. The significance of these antibodies in patients’ circulation so long after the acute infection has yet to be delineated, but could fit the narrative explaining long Covid as a sustained critical inflammatory response.
A prospective cohort study also showed PASC at six months was associated independently with increased convalescent anti-SARS-CoV-2 spike IgG titres and micro-neutralising antibody titres compared with levels at two months post-acute infection.
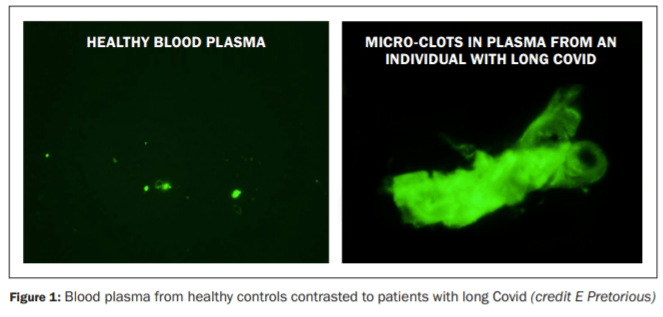
Micro clotting similar to that initially noted in acute Covid-19 has been suggested in long Covid. Plasma from patients with PASC contains both micro-clots and high levels of inflammatory proteins (see Figure 1). The direct effect of these inflammatory proteins and excess fibrinogen in long Covid patients is under investigation.5
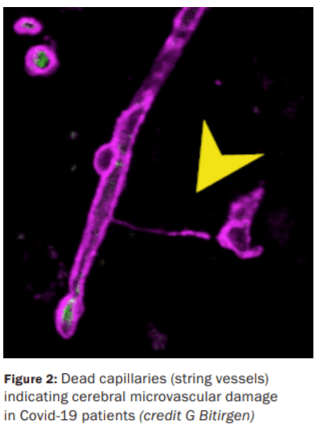
Autopsy studies of cerebral tissue from Covid-19 fatalities have highlighted microvascular brain damage characterised by increased dead capillaries, also known as string vessels (see Figure 2). Using non-Covid-19 control samples, an increase was seen in proteases cleaving NEMO, an endothelial protein found in the brain.7
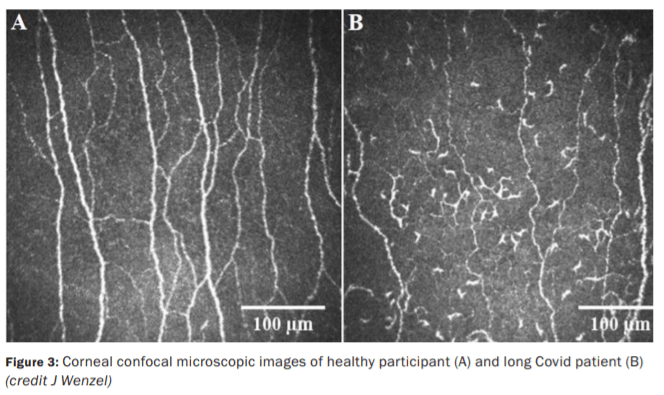
In another study of 40 patients with neurological PASC, corneal confocal microscopy identified corneal small nerve fibre loss (see Figure 3) and increased dendritic cell density in the eyes.1
Diagnostic criteria – including investigations
There is currently a wide variation in how long Covid is investigated. Due to extensive symptoms and variable clinical presentations, a clinic exclusively dealing with long Covid is recommended and has been established at the Beacon Hospital, Dublin, and other centres nationally. Patients should be triaged before arrival, either via electronic or paper form-based assessment, to best investigate and manage individual symptoms.
This pre-consultation evaluation can also direct the need for subspecialist referrals. Considering the increased frequency of neuropsychiatric PASC, routine screening for depression, anxiety and post-traumatic stress disorder (PTSD) is recommended. Current evidence has shown no role for neuroimaging in the event of mental/cognitive impairments alone. Yet specific symptoms like headache and dizziness might benefit from once-off neuroimaging.
In the absence of parenchymal abnormalities or physiological impairments, dyspnoea should be considered in the context of fatigue, deconditioning or dysfunctional breathing patterns. Hyperventilation syndrome is suspected with a high Nijmegen questionnaire score or positive provocation test using end-tidal CO2 monitoring. Respiratory function is usually preserved. In the event of cardiac symptoms, an ECG and rhythm monitor should be done. Cardiology referral, including echocardiogram can be considered.
The role of cardiac MRI is unclear and currently under investigation. There potentially could be a role for acute and convalescent paired serologies in differentiating patients with acute infection, re-infection, and long Covid. Significant differentials to consider will be fibromyalgia and chronic fatigue syndrome, which have overlapping presentations.
Management
Management of PASC continues to evolve. Care plans are currently extrapolated from analogous disease states and non-randomised data. The current best practice is a hybrid model of outpatient care facilitating both virtual consultations and in-person reviews. Ideally, the screening assessment is done electronically to plan a tailored individualised consultation.
Turnbull et al describe a framework for establishing a multidisciplinary PASC service mostly built from experiences with post-intensive care syndrome (PISC).4 It highlights the need for partnership between specialist care and primary care. This partnership has to evolve bi-directional as there is a paucity of longer-term studies on long Covid prognosis. Increasing burdens on primary and hospital outpatients due to Covid-19 restrictions and delayed non-Covid-19 healthcare will contribute to lengthy PASC waiting times as the number of those seeking help increases.
Primary care physicians are more familiar with a patient’s baseline. Hospitals have easier access to complex diagnostic pathways and subspecialist teams. The patient benefits from primary care’s experience coordinating care between multiple specialists, allied health professionals, community therapies, public health nurses and the patient’s family. Hospital-based specialists should liaise closely with GPs to help the patient recover and chart a joint management plan.
Physiotherapy
All long Covid sufferers should be referred to a physiotherapy rehabilitation programme. Physiotherapists in this setting benefit from familiarity with both acute and long Covid or specialist respiratory training. However, many of the principles of long Covid rehabilitation are familiar across the discipline, and workforce considerations may not facilitate subspecialty care.
The key goal is to avoid a delay in rehabilitation and progressive deconditioning. Virtual rehabilitation platforms will likely gain popularity for patients not showing evidence of exercise-induced cardiorespiratory abnormalities, eg, cardiac ischaemia or exercise-induced desaturation. Physiotherapists are also skilled at screening for respiratory PASC beyond physiological impairments.
This can include observing for dysfunctional breathing patterns and hyperventilation syndromes. Hyperventilation syndromes respond well to breathing retraining exercises.
Rehabilitation is initially focused on optimising physical functioning using compensatory strategies. On reaching an exercise plateau, a combination of aerobic exercise and endurance work can help further overcome functional limits. Patients are challenged with increasing intensity of exercises until a supervised overload. The linear progression of a graduated exercise programme is controversial, however. Frequent dips or relapses are common, meaning that exercise tolerance can be variable.
Failure to accommodate this variability can be counterproductive and lead to frustration and risk of disengagement. Functional outcome measurements such as walking distance and visual analogue scale feedback should be used frequently to help motivate and plot disease trajectory
If system capacity allows, it is recommended cardiorespiratory demand is also evaluated. Maximal oxygen uptake and lactate thresholds are the gold standard indices; however, various field tests such as the six-minute walk test have been shown to map these parameters. Intermittent measurement of basic cardiac and respiratory function during rehabilitation exercises will help build an understanding of patients’ individual responses to rehabilitation.
Pharmacological interventions
There are no current evidence-based recommended therapies for long Covid. Pharmacists and other allied health professionals can help by advocating against expensive non-allopathic remedies or cures. Screening for polypharmacy and interactions with prescribed and overthe-counter medications is also helpful.
Social work and employer engagement is crucial as patients are often struggling to return to full-time employment. Inflexible working conditions can hamper recovery as patients cope with the physical and mental sequelae of Covid-19. There is a lack of uniform response as employers come to terms with this emerging clinical syndrome.
We find it notable that a sympathetic and engaged employer approach facilitates a speedier return to full employment. Medical support for a graduated return to work is helpful. A hybrid in-house/work-fromhome model with a graduated return to work is most likely to be successful. Returning too early or unrealistic expectations on either side risks an unsuccessful return and a more protracted overall absence.
Other resources and websites
- NHS website www.yourcovidrecovery.nhs.uk/
- Ireland covid.recovery@beaconhospital.ie
- Long Covid Ireland Support (Facebook group).
- Long Covid Support group (Facebook group).
- UK-based Long Covid-19 Foundation (Facebook group).
Experimental therapies
A range of therapies have been proposed, including melatonin, opiate antagonists, and even hyperbaric oxygen therapy. Patients are sometimes desperate for help and need guidance on the weight of evidence behind any proposed intervention or scientific merit of an unproven approach.
Despite the benefits of vaccinations in reducing the risk of Covid-19 infection, transmission and mortality, vaccines may not reduce post-Covid-19 morbidity. There are multiple anecdotal reports of sometimes dramatic improvement following vaccination. A six-month follow-up of vaccinated patients who contracted Covid-19 showed no apparent benefit from being vaccinated in mitigating PASC.
Previous murine modelling has shown that melatonin can reduce lung injury by increasing apelin 13 expression and reducing reactive oxygen species released during lung injury. Melatonin has shown benefits in lowering delirium in intensive care patients. In sleep studies, melatonin is associated with significant improvement in neuropsychological testing and reduced depression and improved sleep.
Melatonin is potentially helpful for both neurological and respiratory PASC. There is no substantial evidence to support its routine use at the moment, but it is the subject of several ongoing trials.
Therapies for narcolepsy and chronic fatigue syndrome could also have a role in long Covid sufferers with overlapping symptomatology. A holistic approach is probably the safest, pending evidence supporting newer or repurposed therapies.
The future
The pharmaceutical industry is busy trying to meet this evolving event. The recent European Respiratory Society (ERS) 2021 International Congress saw promising phase 1a trial results for LYT-100, a deuterated form of pirfenidone and phase 2 trials are already in progress for respiratory long Covid.
Another dry powder molecule, ASA1125, which has been shown to improve mitochondrial function within the skeletal muscle, will be trialled in patients suffering from muscle fatigue and malaise post-Covid. AT-537, another molecule, is being studied prospectively to evaluate any benefits of the drug on long Covid symptoms after initially being given as an antiviral during acute Covid-19. For now, it appears prevention remains the best bet.
Conclusion
It is essential to follow Covid-19 survivors for as long as they are symptomatic until we understand the true gravity of long Covid. This is a multi-system disease requiring multidisciplinary input. While therapeutic evidence accumulates, patients need significant support and astute use of approaches proven in analogous presentations.
Dr Abhilash Sahadevan and Prof Seamus Linnane see long Covid patients at the Beacon Hospital Post Covid Clinic; covid.recovery@beaconhospital.ie
References
- Bitirgen G, Korkmaz C, Zamani A, et al.
(2021). Corneal confocal microscopy identifies
corneal nerve fibre loss and increased dendritic
cells in patients with long Covid. British Journal
of Ophthalmology, bjophthalmol-2021-319450.
doi:10.1136/bjophthalmol-2021-319450 - Groff D, Sun A, Ssentongo AE, et al. (2021).
Short-term and long-term rates of postacute
sequelae of SARS-CoV-2 infection: A systematic
review. JAMA Netw Open, 4(10), e2128568.
doi:10.1001/jamanetworkopen.2021.28568 - Hellemons ME, Huijts S, Bek L, et al.
(2021). Persistent health problems beyond
pulmonary recovery up to six months after
hospitalisation for SARS-CoV-2; a longitudinal
study of respiratory, physical, and psychological
outcomes. Ann Am Thorac Soc. doi:10.1513/
AnnalsATS.202103-340OC - Parker AM, Brigha E, Connolly B, et al.
(2021). Addressing the post-acute sequelae of
SARS-CoV-2 infection: A multidisciplinary model
of care. Lancet Respir Med, 9(11), 1328-1341.
doi:10.1016/s2213-2600(21)00385-4 - Pretorius E, Vlok M, Venter C, et al. (2021).
Persistent clotting protein pathology in Long
Covid/post-acute sequelae of Covid-19 (PASC) is
accompanied by increased levels of antiplasmin.
Cardiovasc Diabetol, 20(1), 172. doi:10.1186/
s12933-021-01359-7 - Taylor RR, Trivedi B, Patel N, et al. (2021).
Post-Covid symptoms reported at asynchronous
virtual review and stratified follow-up after
Covid-19 pneumonia. Clin Med (Lond), 21(4),
e384-391. doi:10.7861/clinmed.2021-0037 - Wenzel J, Lampe J, Müller-Fielitz H, et al.
(2021). The SARS-CoV-2 main protease Mpro
causes microvascular brain pathology by
cleaving NEMO in brain endothelial cells. Nature
Neuroscience, 24(11), 1522-1533. doi:10.1038/
s41593-021-00926-1












Leave a Reply
You must be logged in to post a comment.