An overview of taking a holistic approach to pain control, as well as pain’s impact on the patient, including its causes and treatment options
In general terms, most people associate pain with some direct cause. It could be from a sports injury, or toothache, perhaps an accident that has resulted in a broken limb. In cases like these, you have an attributable acute pain, which you can then do something about. If it is a toothache, you go to the dentist, the problem gets fixed, and the pain is gone. If it is a broken arm, you go to hospital, have the usual procedures — x-rays, plaster, etc, are carried out and with the right convalescence, the patient returns to normal.
For many though, pain is something which is not acute or for which there is a simple ‘cause and effect’ route to fix the problem. Pain is a constant factor in their lives, something which they manage every day. The reason they have pain may be attributable to one or more different causes; however, it is evident that their pain can have a wholly debilitating effect, not just on their quality-of-life, but also for those around them. This is chronic pain.
The 2006 National Disability Survey Ireland (CSO, 2008) stated that pain was one of the most common disability types reported. Almost 50 per cent of individuals reported pain as the main cause of their disability and of those, 34 per cent indicated arthritis as being the most common cause of injury or illness. Almost 20 per cent stated the pain disability was caused by an accident or injury.
The Pain in Europe survey, published in 2006 by Harald Breivik, indicated for Ireland that:
- 13 per cent of the Irish population and 27 per cent of Irish households were affected by chronic pain.
- 21 per cent of people with chronic pain reported pain so severe they sometimes wish to die.
- The average age of individuals with chronic pain was 48, with only a slightly higher gender bias towards women (W 52 per cent – M 48 per cent).
- The average duration of chronic pain was 4.9 years, although almost 20 per cent of individuals with chronic pain had experienced it for >20 years.
- Almost 70 per cent of individuals with chronic pain reported pain on a daily basis.
- 34 per cent felt pain impacted on their employment.
- 15 per cent of sufferers reported losing a job due to their chronic pain.
- 19 per cent were diagnosed with depression due to chronic pain.
What is chronic pain?
Chronic pain can be defined as pain which has lasted longer than what would be considered as a ‘normal’ healing time, perhaps as part of recovery from illness or injury – generally more than three months. Chronic pain may be attributable to an event, such as an accident, developing from acute pain. Opinion differs as to whether previous acute pain is always the root cause of chronic pain or simply appears, sometimes without an initial cause. In some cases, especially in relation to sports injury in contact sports, the underlying chronic pain may appear some time after an event. Pain may also be related to another condition. Surveys show that in Ireland, 35 per cent of reported chronic pain was arthritis-related. It may be site-specific, ie, back, knee, and wrist, however, 80 per cent of sufferers in Ireland report that their pain relates to more than one site.
For many though, pain is something which is not acute or for which there is a simple ’cause and effect’ route to fix the problem
Types of chronic pain
Pain can be classified either by type of pain, or by body region. Classes of pain types include:
- Nociceptive pain: Aching, boring, worse on movement, anatomically defined, fluctuates in severity.
- Neuropathic pain: Burning sensation, sharp stabbing type, tingling, transient limb pain (shooting), associated with allodynia (experience of pain from a non-painful stimulation of the skin, such as light touch), hypersensitivity, or other sensory changes.
- Mixed nociceptive and neuropathic pain: Combination of symptoms.
- Visceral pain: Dull, non-specific, difficult to pinpoint.
- Autonomic symptoms: Physiological changes (colour, temperature), sweating.
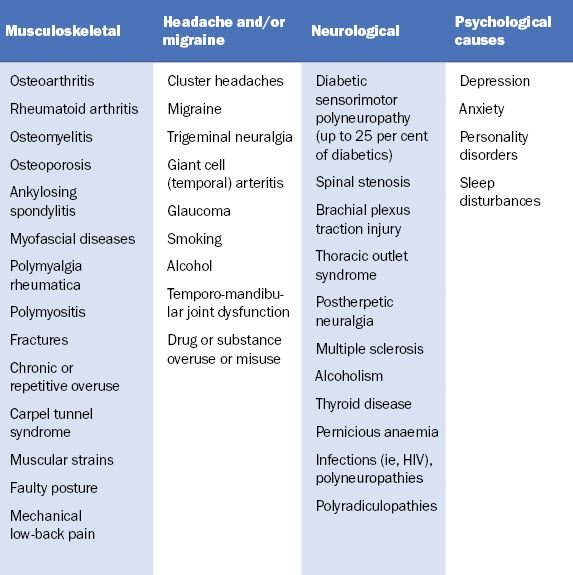
Causes of chronic pain
The cause of chronic pain is often difficult to determine and there are often many aspects to consider. It is this indeterminate nature that can present the biggest obstacle to health professionals to establishing proper diagnosis of the condition. Chronic pain can be attributed to a wide range of identifiable causes – acute injury, arthritis, migraine, or fibromyalgia,
for example. A general classification is detailed below.
Other causes
Chronic pain may arise from anatomical site-related general medical conditions. Site-specific pain includes:
- Abdominal (ie, peptic ulcer, irritable bowel syndrome, pancreatitis, hernias, diverticular disease).
- Gynaecological (ie, endometriosis).
- Obstetric (ie, symphysis pubis dysfunction).
- Urological (ie, interstitial cystitis).
- Cardiovascular (ie, ischaemic heart disease, coronary heart disease, angina, peripheral vascular disease, etc).
- Chronic pain may also result from disease conditions including:
- Rheumatological – conditions such as rheumatoid arthritis, osteoarthritis or fibromyalgia.
- Endocrine – conditions such as hypothyroidism (joint pain), diabetes.
- Infectious – diseases such as hepatitis C, postherpetic neuralgia.
- Malignancy – cancer pain and pain from treatment (ie, radiation, chemotherapy or surgery) [Source: Warrell et al (2004); BMJ Best Practice (2009)]
Treatment
Before moving on to treatment, it is worth noting that, according to figures from the Pain in Europe study (Breivik et al, 2006), 40 per cent of respondents, when asked to describe their care, said it was “inadequate”. Leading on from that, there is substantial evidence based on World Health Organisation (WHO) figures that chronic pain is massively undertreated across the globe. This is due to a variety of factors, such as access to medicines and specialist help.
Another contributing factor comes from sufferers themselves. Individuals with chronic pain often do not seek help for their pain. This occurs for a variety of reasons, including religion, fear, finance, culture and a feeling that healthcare professionals may feel the individual’s pain is ‘imaginary’. Indeed, the fear of stigma and disbelief, especially with females, is the most common reason in Ireland for not seeking help with chronic pain. The most common groups at risk of under treatment for pain are:
- Elderly.
- Female.
- Individuals with emotional or cognitive dysfunction.
- Individuals who do not speak English as a first language.
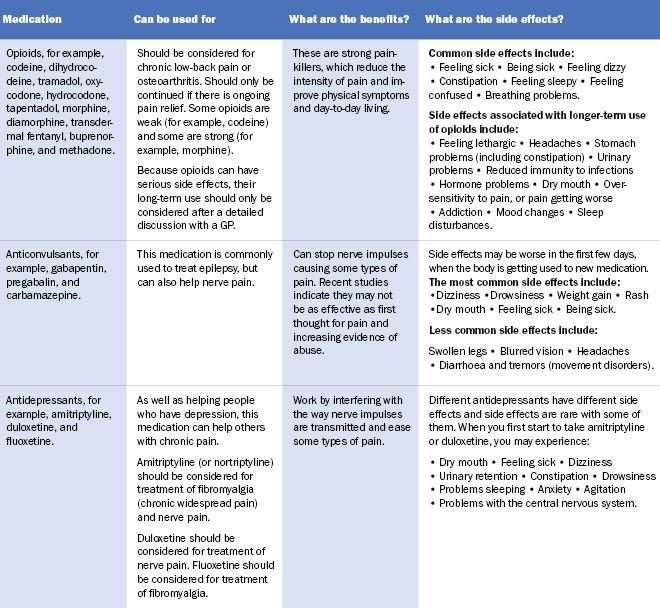
Medication
A successful outcome from GP visits should be a pain management plan. It is highly likely that as part of this, some form of pain-relieving medication will be prescribed. Ideally, advise on promotion of self-help, self management, and other treatments to help improve their condition and add value to the benefit offered by medication. Given the wide and varied nature of chronic pain, there can be a myriad of medication options. The effectiveness of medication depends on the nature and severity of the pain. Types of medications, their benefits and potential side effects are shown in the table below. Regarding treatment of chronic pain caused by headache (ie, migraine), in addition to standard paracetamol and NSAIDs, triptans are considered the most effective way to combat acute attacks if ordinary analgesics do not work. These include:
- Almotriptan.
- Frovatriptan.
- Sumatriptan.
- Zolmitriptan.
- Eletriptan.
- Naratriptan.
All of these are prescription-only medicines, apart from sumatriptan, with an over-the-counter (OTC) version recently becoming available in Ireland.
Self-help
Pain management programme
The pain management programme (PMP) is a psychologically-based rehabilitative treatment for people with persistent pain. It is delivered in a group setting by a multidisciplinary team of experienced healthcare professionals working closely with patients. The main aim is to teach a group of patients with similar problems about pain, how best to cope with it, and how to live a more active life. Referral to a PMP is usually through the GP to the local pain clinic. There are public PMPs in a number of hospitals including:
- St Vincent’s University Hospital, Dublin.
- Tallaght University Hospital, Dublin.
- The Mater Misericordiae University Hospital, Dublin.
- Mercy University Hospital, Cork.
Physical therapy
Physical therapy covers a number of different treatment types, which can be beneficial for chronic pain, especially pain due to musculoskeletal disorders.
- Hot or cold (ice) pack treatment.
- Ultrasound.
- Peripheral nerve stimulation/transdermal electronic nerve stimulation (TENS).
A chartered physiotherapist can help with manual therapy, which helps to increase tissue extensibility and range of movement, thereby decreasing pain. Manual therapy can also help with alignment and joint mechanics issues, which in itself can also help alleviate pain.
Therapeutic exercise – Such as hydrotherapy, can restore joint movement and flexibility and strengthen and condition muscles to help movement, thereby reducing pain.
Medication-overuse headache is the third most common cause of headache after migraine and tension-type headache
Patient education – Can support physical therapy in a self-help or home-based manner. Reading and learning about their condition can assist in management of their own pain.
Exercise – Staying active can be key to improving chronic pain symptoms. Any activity that increases mobility can have not only a positive physical benefit, but also an affirming mental health benefit also.
Cognitive behavioural therapy (CBT)– CBT is a proven ‘talk therapy’, the primary aim of which is to help recognise and manage negative thinking or unhelpful beliefs that lead to increased distress. Generally delivered on a one-to-one basis, the participant is taught techniques and strategies to enable them to challenge their thoughts and change their attitude, leading to a change in future behaviour. Through regular attendance, confidence builds, leading to positive goal-setting. These goals should relate to achieving resumption of activities previously restricted by pain.
Learning problem-solving strategies and stress reduction techniques will help achieve a successful outcome.
Over-the-counter painkillers: Chronic daily headaches and codeine risks
Taking painkillers for longer than 15 days (three days for codeine) runs the risk of medication-overuse headaches. The headaches caused by painkiller overuse last an average of four or more hours. After taking a painkiller for headaches for a prolonged period of time, the body becomes used to the painkillers. A ‘rebound’ or ‘withdrawal’ headache then develops if the patient does not take a painkiller within a day or so of the last dose. The patient thinks this is just another headache, and so takes a further dose of painkiller.
When the effect of each dose has worn off, a further withdrawal headache develops, and so on. A vicious cycle develops as the sufferer gets headaches every day or most days and then ends up taking more painkillers, which only makes the headaches worse. Unless the overused painkillers are stopped completely, the headaches are likely to continue. This phenomenon only seems to occur when taking painkillers for headaches; it does not seem to occur when taking painkillers regularly for other conditions, such as arthritis.
Medication-overuse headache is the third most common cause of headache after migraine and tension-type headache. About one-in-50 people develop this problem at some time in their life. It can occur at any age, but is most common in people in their 30s and 40s. It is more common in women than men. The headache of medication-overuse headache is often described as ‘overwhelming’ and tends to be worse first thing in the morning, or after exercise. It may be a constant ‘dull’ headache, with spells when it gets worse. Codeine is the most common cause of chronic daily headaches. Codeine-based medicines can bring on chronic daily headaches after only three days of use.
How to know if a patient is addicted to codeine
Addiction to codeine can occur by taking OTC remedies containing codeine for longer than the recommended three days. If a patient answers ‘yes’ to any of the following questions, they may be addicted to codeine.
- Do you feel you need to take the codeine products for longer time periods than instructed on the box?
- Do you find yourself buying more and more pills?
- Do you feel you need to take more than the recommended dose?
- Do you start to feel unwell when you stop taking the medicine but feel better when you start taking the medicine again?
These symptoms will not occur if they follow the recommended dosage instructions written on the medicine box.
References on request













Leave a Reply
You must be logged in to post a comment.