Anaesthesiologists are currently playing a vital role in intensive care units in the fight against Covid-19. President of the College of Anaesthesiologists of Ireland Dr Brian Kinirons speaks to Paul Mulholland about why, despite the risks, morale among anaesthesiologists is high
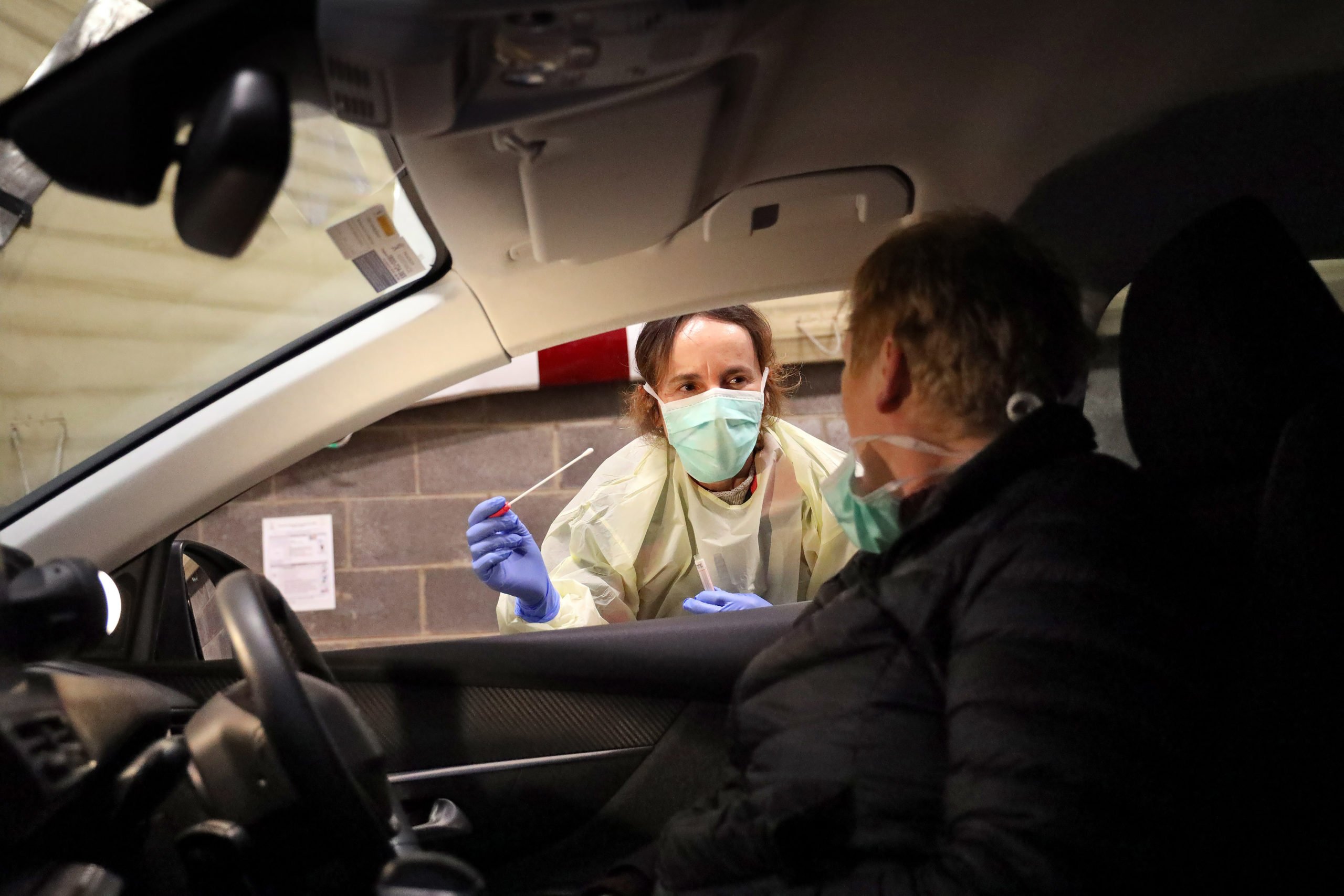
The risk Covid-19 poses to healthcare workers has been one of the dominant themes in media coverage since the pandemic began. This risk particularly applies to those working with the most critically-ill patients in intensive care units (ICUs).
In Ireland, 98 per cent of clinicians working in ICUs are anaesthesiologists. For Covid-19 patients who suffer from acute respiratory distress, anaesthesiologists are responsible for intubation, which allows the patient to be placed on a ventilator.
The intubation and extubation processes carry high risks for healthcare professionals. Not only is the anaesthesiologist carrying out the procedures at the risk of droplet exposure due to close proximity with the patient’s mouth, the production of aerosols of respiratory secretions carry an increased risk of transmission.
This means it is absolutely essential that anaesthesiologists have adequate personal protective equipment (PPE) in order to safely carry out their work. The difficulty in securing PPE since the crisis began has been much commented upon, with a portion of the first batch of equipment the HSE recently procured from China not suitable for use in a healthcare setting.
However, in an exclusive interview with the Medical Independent (MI) on 7 April, President of the College of Anaesthesiologists of Ireland and Consultant Anaesthesiologist in University Hospital Galway, Dr Brian Kinirons, said in his experience to date, PPE for anaesthesiologists had been adequate and he has not heard of any shortages.
“There’s been a lot of concern nationally and it’s been articulated in the papers about PPE,” he told MI.

“I’m in constant communication with our frontline community in Ireland, and as I myself am on the frontline, I’m currently working in a Covid ICU and I use PPE on a daily basis. At a local level, there has been no shortage of PPE. Again, speaking to a wider community, I’m very conscious of the risks of exposing our healthcare workers, and I don’t hear voices coming back to me saying this is a huge problem in individual hospitals.
“I’m very conscious there was a big consignment recently imported. It was a challenge for the Government because the market is saturated in terms of demand and getting the material in itself is difficult and there were concerns, not necessarily about the quantity, but about the quality of the material. All I can tell you is that there seems to be adequate PPE at a local level and I haven’t heard any hospital say that they’ve run out of PPE. It is critical because we are asking our frontline workers to go into close proximity every day, the nurses particularly. The exposure is much, much higher for nurses than doctors, who tend to move on to the next patient.”
Dr Kinirons said it would be “catastrophic” if a large number of doctors and nurses are lost to the frontline during the pandemic. As of 11 April, 2,489 cases of Covid-19 infection were associated with healthcare workers.
Speaking about anaesthesiology, Dr Kinirons acknowledged that it is a “high-risk specialty”.
“We certainly as a College would be very supportive of having good, appropriate PPE for all high-risk interventions,” he said. “We’re a very high-risk specialty because our interventions tend to be things like intubation and extubation, bronchoscopies, and procedures like that. They would be described as aerosol-generated procedures. As interventions that are in the high-risk category, that mandates full PPE, which is currently being provided, as far as I can see, throughout the country.”
Commendable reaction
Dr Kinirons said that the lung injury produced by Covid-19 is not particularly unique. What is unique, and what has caused the current crisis, is the volume of people infected by the virus. This can produce an overwhelming strain on the healthcare service, as seen in northern Italy. However, Dr Kinirons was very positive about Ireland’s reaction to the pandemic so far.
“I think the HSE and the Department of Health are to be commended for their actions in relation to Covid-19,” he said.
“I think no healthcare system is ready for a pandemic and I think at a national level, the HSE has shown a capacity for decision-making and leadership which has been very, very positive. Certainly in my experience locally, and even at a national level, as I sit on national tables, I very rarely have seen such cohesion, such resolve and such common purpose, and this breakdown of silos of practice within the key settings, so I think it has been a very cohesive, focused workforce.”
Dr Kinirons referred to how the pandemic has necessitated changes in the “scope of practice” of healthcare workers.
“In other words, in order for us to manage surge capacity, we need to bring people into ICU who weren’t necessarily familiar with ICU. It might include recovery nurses, it might include anaesthesia, it might include theatre nurses, and all of these groups have stepped up to the mark and engaged in comprehensive upskilling within the ICUs in preparation for this. There’s been a huge buy-in. That would be my experience and I think that’s not exceptional to my hospital. I think there has been a buy-in on a national level and that is manifest in the fact that all the focus now is on surge planning, to the point where, of course, elective surgery has been cancelled and the energy and focus of most acute hospitals is on how to manage the surge.”
ICU capacity
Ireland’s lack of ICU capacity was extremely concerning in light of how northern Italy’s health service, which had a much higher number of ICU beds per head of population, was totally overwhelmed by the spread of Covid-19. Part of the reason for the huge number of deaths in the region is attributable to the fact that ICUs were extended beyond capacity and critically-ill patients were unable to access ventilation.
Again, Dr Kinirons said Ireland’s preparation for the pandemic, in terms of increasing ICU capacity, is worthy of praise.
“There’s a common vision, a common purpose backed with financial support which makes these things happen. The fact that we’ve gone from 240, which is an under-resourced national care network, to over 500 beds just reflects huge credit on the local facilities and they are seeing where they can increase surge capacity. At the moment, the capacity surge is largely Dublin, so the pressures are largely Dublin-based. It’s not to say the other units outside Dublin don’t have patients in a critical state; they all do, but they’re not under the same degree of pressure.”
Dr Kinirons also pointed out how the College of Anaesthesiologists was requested by the HSE’s critical care programme to redeploy doctors on its training scheme to the areas of greatest need.
“Recognising the problem currently in metropolitan Dublin, we made approaches to various hospitals,” he said.
“These are largely model 2 hospitals which don’t have critical care, and also obstetric and paediatric hospitals, which have an absolute degree of capacity based on the fact that they don’t have elective surgery.
“The hospitals, the chairs of departments and the CEOs have been very supportive of this. Again, this is a reflection of that common fighting spirit I’ve talked about. It has allowed people, not just to move within groups, but in actual fact to move doctors across groups. What we’re doing is moving our most precious resource, our doctors, to the areas of greatest need. That could have been very bureaucratically difficult, but it was made relatively easily and it was done within a very short space of time too.”
Dr Kinirons said the steps taken by the Government and health service after seeing the devastating effects of the virus in northern Italy have been vital in bracing hospitals for the pandemic.
“The Government was very proactive in that time. At a national level and at local level, what was happening was capacity planning and a huge part of that was education and training. From my discussions with colleagues around the country, there was a huge amount of emphasis placed on, for example, training staff on the donning, and equally the doffing, of PPE.
“A huge amount of energy and effort went into that. Not only that, but also around pieces like intubating or extubating the Covid-positive patient. In light of this, hospitals around the country seemed to engage heavily in this sort of training prior to our surge. I would say that there is good knowledge out there, that we had the time to do these things, and that it was happening at a local level, a departmental level and within the critical care and nursing community. A lot of that happened as simulated exercises, so there was a lot of education happening within that time. I would be pretty happy with what I’ve seen in terms of the standard.”
Overall, Dr Kinirons said he is “hugely proud” of how his colleagues have “stepped up” in face of this unprecedented challenge, noting how everyone’s working life has changed “irrevocably.”
“For example, we now have a sort of 24/7 consultant cover,” he explained.
“In many units around the country, consultants are living in the critical care units on-call. This was not a negotiated contractual issue, this was just based on the fact that there was a need and that this was the right thing to do. So people ‘living in’ in the hospital isn’t something that has happened before but this is, again, certainly in my specialty, stepping up to the plate. I find on a local level, it has changed everything. Certainly we don’t do any elective work and there is a degree of urgent surgery which will probably move to the private sector. In terms of our focus, everything I do is in critical care. This week, I’m working from 4pm to midnight and the weekend. Next week I’ll be working from midnight to 8 am. So the way we work is completely different.”
Working with PPE also presents unique challenges.
“It is necessary for protection but it is actually a difficult thing to work in,” according to Dr Kinirons.
“It’s uncomfortable, it can get hot, you don’t have freedom of movement and you’re trying to do things for patients which you would normally do without the restrictions of PPE. So it makes doing simple things a little more difficult and of course your capacity to stay in PPE is time-limited as well. You can’t stand for eight hours in a PPE suit; you need time out and you need time off as well. As I said before, what I see at the coalface is cohesion and a system that is working together and that’s everything from radiology to nutrition, to nurses to critical care doctors from our College. There’s a willingness to do the right thing and there is a common perception in pulling together and that doesn’t happen too often.”
Ethical decision-making
Dr Kinirons said that, at the time of writing, the surge had not occurred in the western region, and there was still capacity in the system. However, he acknowledged that this could change, which would put pressure on clinicians in a number of ways, including the need to make difficult decisions about who gets treatment. With this in mind, the College has pointed members towards two Department of Health documents. The first document is The Ethical Framework for Decision-Making in a Pandemic. The second is Ethical Considerations Relating to Critical Care in the Context of Covid-19.
Regarding the second document, Dr Kinirons said: “It reinforces things like a duty of care to the patient, the broader public duty of care and it talks about situations where capacity and resources may be limited, or potentially overwhelmed if there was a huge surge.”
He said that the steps Ireland has taken to ‘flatten the curve’ of infection and reinforcing acute care will hopefully prevent a situation developing similar to northern Italy. The guidance documents are most relevant when demand for services exceeds capacity.
“I think these documents are useful; I think they’re good and they do inform decision-making, there’s no question about that. The trajectory we’re going on would seem to be slightly different to that in northern Italy, so I would have been much more confident that the population changes that we’re seeing in terms of at national level are having a [positive] effect.”
Dr Kinirons also pointed out that ethical decision-making in critical care is not new for physicians working in the area.
“It’s something that has been happening ever since the introduction of critical care; if we go back to the hospital setting, decisions are made on a daily basis about whether resuscitation is appropriate or inappropriate,” according to the College President.
“So it’s not to say that decisions are not made on an ethical basis on a daily basis; they are. I guess the pandemic is about decision-making with a resource which is overwhelmed. And I go back to saying again, everything that we are working for is to prevent the system from being overwhelmed. We’ve doubled, if not more than doubled, our critical care capacity in the space of two-to-three weeks. That’s a remarkable achievement.”
Wellbeing
It is not only the physical health of clinicians that is threatened by the virus — there is also concern about the mental strain of being on the frontline in the middle of a pandemic. Dr Kinirons acknowledged that many doctors are “anxious” about the current situation. But he also stressed the camaraderie and sense of purpose that has characterised the reaction of medical professionals to the pandemic.
“There is a degree of anxiety, no question at all about that,” according to Dr Kinirons, “my sense is that even more so before [the pandemic was declared]. The analogy I heard used, which I thought was quite a good analogy, is that you’re looking out to sea and you know there’s a tsunami coming your way; you can’t see it, but you know it’s out there. I think in a funny way, once we got into this, it was probably a little bit better. I would say the morale among the critical care physicians I’m working with is very good, and I’d say that’s the trainees as well as the consultants.
“What I’m seeing at the coalface, what I’m hearing within the wider community, is very positive, a community which is engaged, keen to actually make a difference and to fight this pandemic. I do accept we could possibly be in this for a while, so this is a marathon rather than a sprint. And I’m very conscious that welfare and health and wellbeing are central to what we do as a College, particularly for the training group and also for our fellows and consultants as well.”
Dr Kinirons said that in addition to its own services, the College has pointed members in the direction of wellbeing supports provided by the HSE, the RCPI, the RCSI, the ICGP, and the College of Psychiatrists.
“But I’m also very conscious that part of the health and wellbeing is for people to be well rested, they need to eat, they need to drink, they need down-time and it’s important that we ensure that those pieces are in place. It’s so important that people get a chance to recover because they are at the coalface and are hugely impressive, from my perspective, in their commitment to providing the best patient care possible in the face of this exceptional demand.”
Dr Kinirons said the College of Anaesthesiologists trainees (CAT) group plays an important role in supporting the specific needs of trainees.
“What’s remarkable is — again, this is anecdotal — the trainees I spoke to were actually very supportive of having to move to an area of greater need from an area of lesser need,” he said.
“It suggests that they are motivated and that morale is good. It’s not something we take for granted and it’s something we need to work on, particularly if this is a longer-duration event. We will have to ensure that they are looked after, that they’re minded. They also referenced that the Medical Council is very good and has been extremely supportive of the trainees.”
Dr Kinirons referred to how the College has cancelled exams, which can be a source of stress for trainees.
“These exams are ‘progressional’ exams, but we’ve taken the view that we would rather a liberal interpretation and they would not stop progression because they didn’t access an exam that they were due to sit, and we will continue to progress them irrespective [of the current situation]”, according to Dr Kinirons.
“They all engaged in training and achieving modules, and we have suggested to them that we would take a very liberal interpretation of module competences during the Covid-19 pandemic so that they are not worried about achieving modular goals at College level. We try to encourage them to communicate with us at the College and to communicate within the CAT group. We’ve had doctors within that group who’ve been off on isolation for 14 days due to inadvertent contact, but the theme of my message is that the College remains open, that we’re here for them, that we’re here to support them, and that is really our function.”












Leave a Reply
You must be logged in to post a comment.